Treatment of dermatitis in children 3 years. Tips for moms: how to recognize and cure dermatitis in a child
Local inflammation of the skin, caused by various reasons, is called dermatitis. This disease occurs very often, it is diagnosed in 80% of babies with skin diseases. Dermatitis in children is often due to the imperfection of the immune system of babies, as well as insufficiently high-quality skin care for the child. Let's figure out what are the symptoms and treatment of this disease.
Noticing redness or a rash on the baby's skin, parents should be wary. It is possible that these are signs of dermatitis. This disease is caused by many different causes, so it occurs very often.
Children under three years of age are at risk for dermatitis. At an older age, this disease also occurs, but somewhat less frequently. Let's figure out what dermatitis is and what are the causes and treatment of this disease.
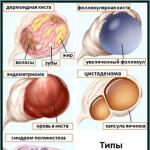
Kinds
Any inflammation of the skin is dermatitis, but the nature of this disease is completely different. Chemical, physical and biological factors, as well as their various combinations, can affect the development of the disease. Dermatitis in a child can be:
- or . These are two different types, but they are caused by one factor - an inadequate response of the immune system to interaction with any substance or group of substances. One of the varieties of this group of diseases is the toxidermic form, its development is provoked by substances that first enter the gastrointestinal tract, and from there into the bloodstream.
- . Called by direct impact on the surface of the body. The impact can be of a different nature.
- . A special type of ailment that affects the skin in places of a large accumulation of sebaceous glands. One of the reasons for the development of seborrhea is the uncontrolled reproduction of an opportunistic fungus that feeds on the secretion of the sebaceous glands.
Advice! Conditionally pathogenic is the microflora that is present on the skin of healthy people. Under certain circumstances, microorganisms begin to multiply uncontrollably, which leads to the formation of inflammation.
- . Dermatitis in children can be viral, bacterial or fungal in nature.
What causes?
Before starting to treat dermatitis in children, it is necessary to identify what causes it was caused. Without the elimination of provoking factors, it will be difficult to achieve success in treatment. All reasons can be divided into two groups - external and internal.

Advice! A combination of factors can cause the development of allergic dermatitis in children. That is, the irritating substance enters the body from the outside, but the inflammatory reaction is caused by an internal factor - an inadequate response of the immune system.
Causes of the atopic form
Atopic dermatitis in children is not uncommon. The exact causes of the development of this disease have not been studied in depth, but the factors that increase the risk of developing this disease are well known. First of all, it is heredity. Cases of atopy often occur in blood relatives.
At the gene level, a tendency to hypersensitivity of the skin is transmitted. In sick children, the content of immunoglobulin E is increased in the blood, this substance provokes the development of allergic inflammation of the skin. External factors that can trigger the development of dermatitis in children
- malnutrition, the inclusion of allergen products in the diet;
- poor skin care;
- nervous tension;
- chronic infections and diseases of the gastrointestinal tract;
- parents smoking, etc.

Causes of the toxidermic form
Toxidermic dermatitis in children is caused by the following reasons:
- food allergens. This is the most common cause of childhood dermatitis in infants and toddlers;
- poor ecology, constant inhalation of air polluted by car exhausts or industrial emissions is one of the causes of the disease;
- taking medications, especially long courses;
Advice! Of course, with drug dermatitis in a child, treatment should not be abandoned, but it is necessary to choose drugs that do not cause negative skin reactions.
Contact Form Reasons
A variety of causes cause contact dermatitis in children, it can be:
- Rare diaper changes, poor hygiene care. If a baby walks in one diaper for a long time, he is rarely washed and bathed, then the risk of inflammation on the skin of the groin and on the legs (in the upper part) is very high.
- Synthetic clothing and underwear. Wearing synthetic clothing can cause dermatitis on the skin of the back, as well as other areas of the body that come into contact with synthetic material.

- Use of unsuitable children's cosmetics (cream, shampoo, bathing foam). Inflammation develops in places where cosmetics were applied to the skin.
- Household chemicals. The cause of dermatitis can be both direct contact with household chemicals, and the use of things that have been washed or washed with powders or gels.
Symptoms
With a disease of any type of dermatitis, the manifestation of the following symptoms is noted:
- redness, swelling, itching;
- blistering;
- the appearance of weeping areas;
- the formation of eczema (in difficult cases);
- crust formation.
Advice! During the period of exacerbation of dermatitis, general symptoms may also appear, children lose their appetite, and do not sleep well. Sometimes the temperature rises.

Let's figure out how dermatitis of different types manifests itself.
atopic
Symptoms of atopic dermatitis in children include:
- dry skin;
- the appearance of severe itching;
- swelling, red spots;
- with the appearance of scratching, erosions can form, with the addition of secondary infections, abscesses form.
Localization of rashes depends on the age of the patient. In babies up to a year, areas of inflammation most often appear on the cheeks. In addition, foci of inflammation are often formed on the inner bend of the elbows. Dermatitis on the elbows and in the popliteal fossae, most often manifested in patients older than 2 years.
Contact
Contact dermatitis appears at the site where the irritant has been in contact. Therefore, the most likely localization of inflammation are the palms. After all, it is with our hands that we most often come into contact with various objects.
So, dermatitis on the palms of a child may appear after the baby strokes a pet or picks up a bunch of wildflowers. Dermatitis on the hands of children is of two varieties:

- Erythematous. It can occur in a chronic or acute form. The main symptom is redness and swelling of the skin on the palms. Later, blisters filled with a clear liquid form. When the blisters burst, crusts form.
- palms is characterized by the formation of painful seals, the liquid in these blisters is absent or located deep under the skin. This form of dermatitis on the palm is noted in older children, the cause of the formation of blisters is a mechanical effect, for example, when doing some kind of work.
In addition, contact dermatitis can occur on any part of the body where the skin has been in contact with the irritant. So, after walking through a flowering meadow, dermatitis on the legs may appear due to contact with certain types of plants.
Dermatitis on the back of a child can occur when wearing synthetic clothing. On the elbows of a child, contact dermatitis often occurs when low-quality cosmetics are used. But inflammation in the groin and between the legs, most often, is associated with insufficient quality hygiene care.

seborrheic
This type of skin disease most often appears on the scalp, as there are many sebaceous glands. Crusts form on the head (hairy part), itching occurs.
Advice! The appearance of seborrheic crusts on the head of a baby in the first months of life is considered a variant of the norm. In this case, the child does not require special treatment, it is enough to provide special hygienic care.
If seborrhea is severe, then the skin of the face can become the affected area, most often the forehead - near the eyebrows and along the hairline.
perioral
With this type of disease, rashes appear on the face of a child. Papules and pustules form around the lips and wings of the nose. Rarely, rashes can be seen on the cheeks and chin. The disease can occur from climate change, with a weakened immune system, the use of inappropriate children's cosmetics.

Treatment
This question is of interest to parents of sick babies. However, it is impossible to give an unambiguous answer to it, since the disease has a different nature and requires a different approach to treatment. Only a doctor can answer the question of how to treat a skin disease after a diagnosis and a thorough examination of the child.
Only a general treatment regimen can be given here. First of all, you need to eliminate the cause, which is the trigger of the inflammatory process in the skin. If it is an allergic disease, then it is necessary to exclude contact with the allergen. In the event that insufficiently good care became the cause, then you need to monitor the cleanliness of the child's skin, change diapers in a timely manner.
Most often, dermatitis is treated at home. Hospitalization is necessary only in the most severe cases. Treatment of dermatitis must necessarily include a set of measures, as a rule, these are:

- The use of medicines. Most often, children's skin ailments are treated only with external means - ointments, creams. If necessary, systemic agents can be prescribed.
- Diet. With inflammation of an allergic nature, a hypoallergenic diet is necessary.
- General strengthening of the body. The child can be prescribed vitamin therapy, recommended sanatorium treatment.
Nutrition
Diet is an important part of the healing process. If the child is breastfed, then the diet is assigned to the mother, she should switch to hypoallergenic nutrition. In the absence of breast milk, it is necessary to choose a hypoallergenic baby food, the choice of an adapted mixture should be discussed with the attending physician.
With a tendency to dermatitis, children need to be extremely careful in introducing complementary foods. You can start feeding only after six months, since at an earlier age the child's digestive system is not ready to digest any food other than mother's milk.

The new product is introduced carefully, the first portion should not exceed half a teaspoon. Older children are recommended a hypoallergenic diet that excludes foods that provoke exacerbations of dermatitis.
Medicines
Only a doctor can decide how to treat dermatitis on the hands or other parts of the body. Without the recommendations of the attending physician, you should not use ointments and creams, especially hormonal ones. As a rule, treatment is carried out with the following drugs:
- Ointments of complex action, relieving itching in dermatitis, as well as stopping inflammatory processes, relieving swelling.
- Moisturizing creams are necessary if dermatitis on the face is accompanied by dry skin. Special therapeutic children's cosmetics are used.

- In the event that the inflammatory process on the skin that affected the back, elbows or face is accompanied by the formation of weeping areas, it is necessary to use ointments that effectively dry.
- Hormonal ointments in childhood are used only in the most severe cases and only as directed by a doctor.
- Sometimes, in order to quickly relieve itching, systemic antihistamines are prescribed.
So, dermatitis in children is quite common. Inflammatory processes on the skin can be triggered by various reasons. In babies, most often, the cause of inflammation is allergies, as well as improperly organized nutrition and poor hygiene care. With dermatitis in children, treatment is prescribed individually.
Atopic dermatitis (allergic dermatitis), diathesis - all these are skin manifestations of allergies, caused by essentially the same thing - allergens, toxins and their interaction with the child's skin.
Atopy is a genetic predisposition to produce excessive amounts of immunoglobulin E in response to contact with environmental allergens. The term atopy comes from the Greek word meaning alien. Manifestations of atopy are various allergic diseases and their combinations. The term "allergy" is often used as a synonym for allergic diseases mediated by immunoglobulin E, but in some patients with these diseases, the levels of this immunoglobulin are normal, and then a non-immunoglobulin E-mediated variant of the course of the disease is isolated.
Dermatitis is an inflammatory skin disease. There are several forms of dermatitis: atopic, seborrheic, contact, etc. The most common form is atopic dermatitis.
Atopic (or allergic) dermatitis, one of the most common skin conditions in infants and children, usually begins within the first 6 months of life and often continues into adulthood. More often sick are children under the age of 1 year, in whose families there are cases of allergic diseases. This chronic skin disease affects 9 out of 1,000 people. Atopic dermatitis is often associated with allergic diseases such as bronchial asthma and allergic rhinitis.
Other terms are often used to refer to atopic or allergic dermatitis. The most common is eczema, even a new term has been proposed: "Atopic eczema/dermatitis syndrome". Previously, such terms as diffuse Broca's neurodermatitis, Besnier's pruritus, eczematoid, constitutional eczema, etc. were widely used. In our country, almost all skin lesions in children were called diathesis. Atopic dermatitis is also called childhood eczema. Atopic dermatitis was included in the group of allergic diseases in 1933 based on the association of this form of eczema with bronchial asthma and allergic rhinitis. Indeed, Atopic dermatitis is most often the first manifestation of this atopic triad. Atopic dermatitis is characterized by a hereditary predisposition to allergies, age-related morphology of lesions, staging of development, and a tendency to a chronic relapsing course.
Atopic dermatitis usually progresses with exacerbations and remissions until adolescence. However, for some people it stays longer. Atopic dermatitis can lead to viral, fungal, and bacterial infections and even eye damage.
Clinical forms of atopic dermatitis depending on age.
Atopic dermatitis is divided into 3 successive phases: infantile (up to 2 years old), child (from 2 years old to 13 years old), adolescent and adult (from 13 years old and older), with different manifestations.
The infantile form of atopic dermatitis is observed in a child from birth to 2 years. Favorite localization of dermatitis: face, extensor surfaces of the limbs, can spread to the trunk. Characterized by weeping, crusting, dry skin. Atopic dermatitis is often exacerbated by the introduction of complementary foods and teething.
Children's form of atopic dermatitis (2-12 years old): skin rashes mainly on the flexor surface of the limbs, on the neck, in the ulnar and popliteal fossae and on the back of the hand. Hyperemia and swelling of the skin, lichenification (thickening and strengthening of the skin pattern), papules, plaques, erosions, cracks, scratches and crusts are characteristic. Cracks are especially painful on the hands and soles. There may be hyperpigmentation of the eyelids due to scratching, the appearance of a characteristic fold of skin under the eyes under the lower eyelid (Denier-Morgan line).
In the adult form of atopic dermatitis, the teenage form (up to 18 years) is distinguished. In adolescence, both the disappearance of rashes (more often in young men) and a sharp exacerbation of dermatitis with an increase in the area of the lesion, damage to the face and neck (red face syndrome), the décolleté and skin of the hands, around the wrists and in the elbow pits are possible.
The adult form of atopic dermatitis often continues into adulthood. An allergic lesion of the flexion surfaces in the area of natural folds, the face and neck, the back surface of the hands, feet, and fingers predominates. Moisture usually indicates the addition of a secondary infection. But in any phase of Atopic dermatitis, dry skin, pruritus, thickening of the skin with increased skin pattern (lichenification), peeling, hyperemia, and rashes typical of each age are typical.
With atopic dermatitis, a vicious circle is formed: itching - scratching - rash - itching. Mandatory criteria for diagnosis include itching, chronic relapsing course, atopy in the patient or relatives, and rashes that are typical in appearance and localization. There are many additional symptoms of atopic dermatitis, not mandatory, but often very striking. The diagnosis of atopic dermatitis depends on the exclusion of conditions such as scabies, allergic contact dermatitis, seborrheic dermatitis, psoriasis, and ichthyosis.
The skin in atopic dermatitis is changed even without exacerbation and on outwardly unchanged areas of the skin. Its structure and water balance are disturbed. This dictates the need for special skin care.
Photo of skin manifestations of atopic or allergic dermatitis








Reasons for the development of atopic dermatitis
The exact cause of atopic dermatitis has not yet been determined, but there are predisposing factors (genetics, food allergies, infections, irritating chemicals, extreme temperature and humidity, and stress). Approximately 10% of all cases of atopic dermatitis are caused by allergies to certain types of food (eg, eggs, peanuts, milk).
Atopic (allergic) dermatitis tends to worsen with increased sweating, mental stress, and extremes in temperature and humidity.
Irritation is a secondary cause of atopic dermatitis; causes a change in the structure of the skin, which eventually leads to chronic damage to the skin.
Factors that play a role in the implementation of atopic dermatitis.
In 80% of cases, the family history is burdened, more often on the mother's side, less often on the father's side, and often on both. If both parents have atopic diseases, the risk of disease in a child is 60-80%, if one has 45-50%, if both are healthy - 10-20%. Endogenous factors in combination with various exogenous factors lead to the development of symptoms of atopic dermatitis.
In the first years of life, atopic (allergic) dermatitis is a consequence of food allergies. Cow's milk proteins, eggs, cereals, fish, and soy are common causes. The benefits of breastfeeding are known, but a hypoallergenic diet for the breastfeeding mother is essential. But in some cases, when the mother herself suffers from severe allergies, it is necessary to use artificial feeding with milk mixtures based on highly hydrolyzed or partially hydrolyzed milk proteins, less often soy mixtures.
With age, the leading role of food allergy in the occurrence of atopic dermatitis decreases (for example, up to 90% of children who cannot tolerate cow's milk acquire the ability to tolerate it - tolerance - by 3 years), and allergens such as house dust mite, pollen come to the fore , mold spores. A special role in the course of atopic dermatitis is played by staphylococcus aureus. It is sown from 93% of affected areas and from 76% of intact (not changed in appearance) skin. Staphylococcus aureus produces endotoxins with superantigen properties and may maintain chronic inflammation in atopic dermatitis.
Symptoms of prickly heat
Outwardly, the signs of allergic dermatitis differ from each other in the nature of the rash.
Prickly heat occurs on the folds of the arms, legs, neck, armpits, in those places where the humidity is high and which sweat more often. The rash with prickly heat is small, pink, does not inflame and quickly passes within 2-3 days. The question is often asked whether there can be prickly heat on the face when the whole child is covered with small pimples, a rash from head to toe - this is not prickly heat, but allergic dermatitis (this is the same atopic dermatitis), although these concepts are similar, and such a rash takes much longer - within a month, subject to a strict hypoallergenic diet and moderate nutrition.
Symptoms of diathesis, atopic dermatitis
Diathesis often manifests itself as redness of the cheeks, peeling, pimples on the cheeks and face and does not spread beyond the face. The reason for diathesis is simple - “they ate something wrong”, this is an instant allergic reaction of the child to a food product and disappears if this allergen is excluded from the child’s menu. Diathesis is not an independent disease, but an infantile stage of atopic dermatitis, and if its manifestations are ignored and not treated, allergic dermatitis will pass into the adult stage.
Rash with allergic dermatitis - small red pimples mainly on the folds and hands of the arms, legs, armpits, on the sides, on the abdomen, on the head, including in the hair, and reddened rough spots around the eyes and on the cheeks, often on the body. The spot of the rash can increase in size and get wet (children's eczema), become inflamed, resembling a pimple or rash with chickenpox, the skin can thicken, crack. The rash is often accompanied by itching, especially at night and after the child sweats. A rash with atopic dermatitis does not go away for a long time even with a hypoallergenic diet, it leaves behind dark spots on the skin.
The main reason for the exacerbation of atopic dermatitis under the age of one year is the same allergen and overeating. An allergy is an overactive reaction of the immune system to a foreign protein. The immune system finds it, produces antibodies that neutralize the allergen - the process is accompanied by an inflammatory reaction. The fact is that the child's enzymes cannot completely break down some substances and they enter the intestines in the form of an allergen. When overeating, not all food has time to decompose into components digestible by the body and it begins to rot in the intestines, toxins appear that are absorbed into the bloodstream and cause an allergic reaction in the body. The immature liver of a child is not able to neutralize these toxins, and they are excreted in the urine, through the lungs and through sweat. With sweat, toxins - allergens - get on the skin, the skin becomes inflamed, atopic dermatitis appears, an infection joins the inflammation.
The liver in a child is one of the most immature organs, but its activity, its ability to neutralize absorbed toxins is individual. That is why not everyone has allergic dermatitis; an adult liver can neutralize almost everything, so adults do not have such problems; atopic dermatitis often resolves with age, due to the maturation of liver cells.
atopic march.
Atopic march is a natural course of development of manifestations of allergic dermatitis. It is characterized by a typical sequence of development of clinical symptoms of atopic disease, when some symptoms become more pronounced, while others subside. Usually symptoms and signs of atopic dermatitis precede the appearance of bronchial asthma and allergic rhinitis. According to several studies, approximately half of patients with atopic dermatitis subsequently develop bronchial asthma, especially with severe allergic dermatitis, and two-thirds develop allergic rhinitis. Children with the mildest course of the disease did not develop allergic rhinitis or bronchial asthma. The severity of atopic dermatitis can be considered as a risk factor for asthma. According to studies, with severe atopic dermatitis, the risk of developing bronchial asthma is 70%, with mild atopic dermatitis - 30%, and in general among all children - 8-10%. Therefore, it is so important that treatment is aimed not only at preventing exacerbations of atopic dermatitis itself, but also at preventing the development of other forms of atopic disease.
The disease negatively affects the quality of life of patients and their families, and also requires considerable expenses. Research has shown that caring for a child with atopic dermatitis is more stressful than caring for a child with insulin-dependent diabetes.
Treatment of skin allergic symptoms and atopic dermatitis
Treatment of prickly heat: do not allow the child to sweat, change the diaper often, wet sliders, maintain normal humidity in the child's room and a temperature regime of 20-21 degrees. At least temporarily remove the oilcloth from under the child's sheet. Bathe the child in a slightly pink solution of potassium permanganate, or add a string infusion to the bath. Lubricate the affected areas with baby cream or sterilized vegetable oil.
Treatment of diathesis - the initial stage of atopic dermatitis - is the exclusion from the child's diet of foods that can cause allergies. Exclusion of the allergen from the mother's menu if she is breastfeeding. Manifestations of diathesis can be lubricated with infusion of string, but better with infusion of bay leaf - it does not dry the skin as much as string. Separate pimples can be lubricated with brilliant green.
The treatment and consequences of atopic dermatitis are very multifaceted and have more nuances. In addition to the fact that the treatment of atopic (allergic) dermatitis is successful only if the recommendations listed above for the treatment of prickly heat are followed, there are additional methods of treatment.
Treatment of atopic dermatitis
Currently, a complete cure for atopic dermatitis is not possible. Atopic dermatitis is a chronic disease that requires long-term monitoring of the course of the disease. An integrated approach to therapy is needed. Treatment consists of selecting the most appropriate combinations of supportive basic therapy (skin care) and anti-inflammatory therapy as needed. Eliminating or reducing contact with the allergen and reducing non-allergenic exposures prevents the exacerbation of allergies. The effectiveness of treatment for atopic dermatitis is significantly increased if the patient, his parents and family are educated in the system of allergy schools.
Since atopic dermatitis is a chronic disease, the success of its treatment requires constant cooperation between the doctor and the parents of a small patient.
The doctor's efforts are aimed primarily at suppressing allergic inflammation of the baby's skin and reducing the effect of allergens. A properly selected diet, with the exclusion of food allergens from the diet, can significantly improve the condition, prognosis and outcome of atopic dermatitis.
The leading physician in children with atopic dermatitis should be a dermatologist interacting with an allergist and other specialists (neuropathologist, gastroenterologist).
External treatment occupies an important place in the complex treatment of children with atopic dermatitis. Its choice depends on the condition of the skin, the area of the lesion and the stage of the disease, and the goals are: suppression of inflammation in the skin, reduction of itching, elimination of dryness, prevention of secondary infection.
The main goals of the treatment of atopic dermatitis.
1. Elimination or reduction of inflammatory changes on the skin and itching.
2. Restoration of the structure and function of the skin, normalization of skin moisture.
3. Prevention of the development of severe forms of the disease.
4. Treatment of concomitant diseases.
5. Prevention of the progression of atopic disease (atopic march).
Treatments for atopic dermatitis follow logically from its causes:
Allergic symptoms are provoked by an allergen, therefore, all potential allergens from the child's menu and around him must be excluded, since allergens also enhance each other's action. Example: you gave a child a cherry - there were no rashes on the skin, but you gave the child a cherry during an exacerbation of atopic dermatitis and the rash spread all over the body with lightning speed. The same applies to fried, sweet. Fatty foods cannot be broken down and absorbed completely, and sugars enhance the fermentation processes in the intestines, poisoning the children's body with toxins. Exclude from the menu for the time of allergic rashes all red vegetables and fruits, berries and juices from them, greens, cereals containing gluten, especially semolina. Nutrition, the diet of a child with atopic dermatitis fully applies to the mother if she is breastfeeding.
Eliminate contact with the allergen.
In the treatment of atopic dermatitis, measures to reduce exposure to allergens play an important role. At an early age, dietary restrictions play a major role.
The diet usually includes the avoidance of eggs and cow's milk, as well as extractives, food additives, preservatives, emulsifiers, fried meats, sauces, carbonated drinks and foods with high allergenic activity (honey, chocolate, cocoa), regardless of whether they were the causative factor or not. At the same time, in about 90% of cases, foods that cause exacerbations of atopic dermatitis are milk, eggs, peanuts, soybeans, wheat and fish. If a food allergen is significant, then eliminating it from the diet leads to significant clinical improvement. But, since almost any product can cause an allergic reaction, the selection of such an elimination diet (diet with the exclusion of certain foods) should be strictly individual and based on proven intolerance to the product. In addition, it is recommended to reduce the amount of salt in food.
Hypoallergenic diet. Sample menu for a child - atopic
breakfast - porridge from unroasted buckwheat (boiled in the third water and soaked for a couple of hours first) + half a teaspoon of oil per gram of 200 porridge.
lunch - puree soup: boiled and slightly mashed vegetables (soaked potatoes, white cabbage, onions, teaspoon vegetable oil) + beef 50 grams, cook for 30 minutes. then drain and cook again until tender.
dinner - millet porridge (gluten-free, it's not wheat!) In short, sort it out, wash it 6 times in cold water, then boil it in the third water. Let me explain: on the 3rd water, it means it boiled, they poured it out and so on 2 times.
Of fruits, only apples, but not store-bought.
All herbs can be allergens and give a cumulative allergy, that is, it will pour out after 3-4 weeks and it is not clear why.
Do not overfeed the child, let him eat slowly, in small portions and chew food well if he is already chewing - so he will be satisfied with less food and it will be completely absorbed. When bottle-feeding, dilute a smaller amount of the mixture in water than is normal, make a smaller hole in the nipple. Sometimes take away the bottle and give again after a while. Any pediatrician will tell you that atopic dermatitis is very rare in thin children.
At an older age, measures to eliminate house dust mite allergens, animal allergens, molds, pollen, etc. from the environment play an increasingly important role.
Some measures should be applied regardless of which allergen is "guilty" in the occurrence of atopic dermatitis. First of all, we are talking about reducing contact with dust, recommendations for cleaning and caring for bedding.
You should not put a computer, TV and other household appliances in the bedroom. In the house where the allergic person lives, it is strictly forbidden to smoke.
Also, children with a tendency to atopic dermatitis should avoid contact with irritants (irritants), including alkaline soaps and detergents, which are part of conventional household chemicals, avoid irritating effects of temperature and humidity factors, fabric structure.
Skip close-fitting clothing and replace it with loose-fitting cotton or blended clothing to avoid overheating. The most important qualities in this case, apparently, are breathability and softness (clothes should not rub!). Two randomized controlled trials found that texture or softness/roughness of the fabric played a greater role in terms of comfort and the absence of skin irritation than the use of natural or synthetic material. Nails should be cut short so as not to damage the skin when combing atopic manifestations.
With regard to such a measure as the use of special anti-allergic protective covers impermeable to allergens, this measure can also be useful to all patients with atopic dermatitis. This is evidenced by medical research data. Thus, in a 12-month study in adults, the use of special protective covers for bedding led to a clinical improvement in the course of atopic dermatitis, even in patients who did not have hypersensitivity to house dust mite. This indicates that such covers reduce contact with a number of factors (with allergens of other groups, irritants, and even, possibly, with bacterial superantigens).
Remove all fur toys, plastic and rubber toys that have even a slight smell. Wash leftover toys often with baby soap.
We have limited the ingress of allergens into the blood, what to do with the existing ones? Since toxins can be excreted in the urine, give your child plenty of water during atopic dermatitis flare-ups. It is better to give water not boiled, but artesian with minerals.
Sorbents will help limit the absorption of toxins from the intestines: enterosgel, sorbogel, smecta, activated charcoal - they are absolutely harmless, are not absorbed in the intestines, and it makes sense to take them to a nursing mother and child.
It is very important for Atopic dermatitis to achieve a stable stool 1-2 times a day for both the child and the nursing mother. Lactulose syrup works well in this sense - dufalac, normase - it can be used even by a small child, it is not addictive, but it is better to start with the smallest dosage and gradually bring it up to the norm recommended for the age group. It is better to give the syrup in the morning on an empty stomach, and also gradually reduce the dose.
Now you need to minimize sweating and skin contact with all sorts of microbes. Maintain the optimum temperature in the child's room of 20-21 degrees and humidity of 60-70%, ventilate more often, change bedding every day. Change your underwear often, it should be cotton, with long sleeves and trousers. As soon as the laundry becomes damp, immediately change it. Wash the things of a child with atopic dermatitis - bed linen (including your own), clothes only in baby powder or with baby soap.
You need to walk more, while wearing a minimum amount of clothing for the child. Clothing should not rub, generally minimize skin contact with outerwear, synthetics, dyes.
Especially about bathing in atopic dermatitis.
Baths do not have a very good effect on the course of atopic dermatitis. Bathing during an exacerbation of the disease is not necessary for long, in warm and only boiled water, or water passed through a good filter - the water should not contain chlorine! You can bathe in a weak celandine, a slightly pink solution of potassium permanganate, in a bath with the addition of sea salt (a little bit). Use soap and shampoo for atopic dermatitis only for children and no more than once a week, so as not to wash off the protective fatty film from the child's skin.
The prohibition of bathing in Atopic Dermatitis is a mistake, but a few simple rules must be followed:
1. Bath or shower should be moderately warm. The optimal duration of bathing is about 20 minutes. It is better, if possible, to use dechlorinated water (filters or settling the water in the bath for 1-2 hours, followed by the addition of boiling water.
2. You can not use washcloths, rub the skin, regardless of whether there are symptoms of allergic dermatitis at the moment. Only high quality, hypoallergenic pH neutral cleansers should be used.
3. In case of exacerbation of atopic dermatitis after bathing, the skin should be blotted with a soft towel (do not wipe dry or rub!) and apply an emollient (Bepanten, Lipikar, F-99, etc.) for 3 minutes.
4. Avoid swimming in pools with chlorinated water. In some cases, negative effects can be avoided by showering with mild cleansers after the session, followed by moisturizing and skin softening preparations.
Medical treatment of atopic dermatitis
Treatment of Atopic dermatitis is prescribed only by a doctor individually, based on the symptoms and nature of the rash.
Some pediatricians advise taking anaferon during an exacerbation of atopic dermatitis. Anaferon has a modulating effect on all key components of the immune system, significantly increasing the production of IFN, which reduces the level of Th 2 (T-helper 2) activation and provides not only the prevention of acute respiratory viral infections, but also helps to lower the level of immunoglobulin E IgE (one of the indicators of the body's allergic mood). ). This was proven in clinical studies of Anaferon for children on a group of children with bronchial asthma.
The role of allergen-specific immunotherapy in the treatment of atopic dermatitis.
Once a causative allergen has been identified, allergen-specific immunotherapy (ASIT) becomes important. The data obtained suggest that ASIT can not only prevent the exacerbation of atopic dermatitis, but also prevent the progression of the atopic march.
What means of systemic (general) action are used in atopic dermatitis?
First of all, antihistamines. Indications for their appointment due to the critical role of histamine in the mechanisms of development of pruritus.
The ETAC study (English: Treatment of the Child with Early Stage Atopy) examined the role of cetirizine (Zyrtec) in preventing the development of an atopic march. Infants were treated with high doses of cetirizine (0.25 mg/kg twice daily) or placebo. The results of the study are not entirely unambiguous, but in general, the use of Zirtek led to a 2-fold reduction in the risk of developing bronchial asthma in children with sensitization to aeroallergens.
Anti-allergic medicines: suprastin, tavegil, diphenhydramine. With severe itching, you can use topical antihistamines - fenistil-gel. Dry skin and cracks are often smeared with bipanthen, dermopanten (cream or ointment).
First-generation antihistamines are prescribed during a period of pronounced exacerbation of atopic dermatitis, when their sedative effect is needed. For long-term use, drugs of the 2nd and 3rd generations are chosen, because. they do not cause drowsiness, dry mouth; there is no need for frequent drug changes.
Systemic antibiotics are used for fever and lymphadenitis, clear signs of secondary infection.
They prefer the group of macrolides and cephalosporins of 2-3 generations.
In especially severe, persistent cases, in the presence of extensive eroded skin surfaces, systemic hormones (glucocorticoids) are used.
Sometimes drugs are prescribed that regulate the function of the nervous system.
In the usual uncomplicated course of atopic dermatitis, in the absence of signs of immunological deficiency, immunotherapy is not prescribed.
External (local, topical) treatment of atopic dermatitis.
Without external therapy, it is impossible to imagine the treatment of atopic dermatitis.
Goals of topical treatment of atopic dermatitis:
1. Suppression of inflammation in the skin and associated main symptoms of acute (hyperemia, edema, itching) and chronic (lichenification, itching) phases of the disease.
2. Elimination of dry skin.
3. Prevention of secondary infection.
4. Restoration of damaged epithelium.
5. Improving the barrier function of the skin.
The use of moisturizers in conjunction with hydration can help restore and maintain the stratum corneum barrier. Elimination of dry skin is the most important part of the treatment of atopic dermatitis.
With exacerbations, external hormonal preparations of topical (local) action are used. Preference is given to the latest generation drugs (Advantan, Elocom). Treatment begins with highly active drugs (3-5 days), and then (if necessary) continue therapy with a less active drug (up to 2-3 weeks).
Good help with external manifestations of allergies (only on the rash itself, without eliminating the causes of dermatitis) corticosteroid hormonal ointments and creams. Corticosteroid hormones of the latest generation are relatively safe and have a minimum of side effects due to the fact that they are practically not absorbed into the systemic circulation, they have been used for atopic dermatitis since six months. This, for example, elocom, advantan. When wetting, it is better to use the form of a cream, for dry skin and cracks - ointments. It is not worth abruptly canceling hormones, gradually reduce the dose of the drug, mixing the hormone cream with baby cream, ointment with bipanthen.
You can not use fluorinated hormones in children of the first years of life, as well as in all patients - on the face, neck, in natural skin folds and anogenital area due to the risk of skin atrophy.
Hormonal external agents are absolutely contraindicated:
1. in tuberculosis, syphilitic and any viral process (including chickenpox and herpes simplex) at the site of application of the drug,
2. with a skin reaction to vaccination at the site of application of the drug,
3. with hypersensitivity to the components of the drug.
Reasons why treatment with topical hormonal drugs may not be effective:
1. ongoing contact with the allergen,
2. superinfection with Staphylococcus aureus,
3. inadequate drug activity,
4. insufficient use,
5. non-compliance with the treatment regimen,
6. reaction to the components of the drug,
7. rarely - insensitivity to steroids.
In addition, during exacerbation of atopic dermatitis, various lotions, wet-drying dressings, disinfecting liquids (fucorcin, Castellani liquid, methylene blue, brilliant green) are used. When a secondary infection is attached, there are ready-made forms of external antibiotics (tetracycline ointment), antifungal agents (candida, clotrimazole) and their combinations. For deep cracks, drugs are used that affect the regeneration and microcirculation processes in the skin (zinc ointment).
A new drug and a new approach to external therapy of atopic dermatitis.
Despite the effectiveness of steroids, their use, especially in areas with thin skin (face, neck, natural folds, anal area, external genitalia) can cause a number of side effects: skin atrophy, development of striae, telangiectasias (dilated small blood vessels), etc. d. If the affected area is very large, then the use of steroids can cause a systemic effect. Therefore, topical non-hormonal drugs are being developed.
Currently, such a new non-hormonal topical drug is Elidel (pimecrolimus 1% cream). It belongs to a new class of calcineurin inhibitors (blocks a special enzyme in T-lymphocytes responsible for the production of inflammatory mediators). It penetrates well into the skin, but practically does not penetrate the skin into the systemic circulation. Its use is allowed from the age of 3 months, and it does not cause the formation of striae, telangiectasia and skin atrophy. In addition, in terms of itch relief, the drug shows a faster effect than corticosteroids.
A new strategy for the treatment of an exacerbation of atopic dermatitis based on Elidel has been proposed, in which moisturizing and softening agents are used as a permanent supportive treatment, and at the first, earliest signs of an impending exacerbation of allergic dermatitis, Elidel treatment is started 2 times a day, and only in severe cases. exacerbations, topical hormonal preparations are used.
In the latter case, after a course of topical hormones, Elidel is used to continue treatment after the process subsides to moderate and continues until the exacerbation subsides, and in the future it is recommended to use it when the first symptoms of atopic dermatitis appear. Studies have shown that such a strategy can prevent the progression of an exacerbation to a severe one, in the treatment of mild and moderate exacerbations, the use of hormonal drugs can be dispensed with altogether, and with the help of an early use strategy, control of the disease can be achieved. The new strategy is expected to be a long-awaited opportunity to interrupt the progression of the atopic march. Unfortunately, the drug is not cheap. But now he has taken a strong place in the treatment of manifestations in areas with sensitive thin skin.
Physiotherapy and phytotherapy in the treatment of atopic dermatitis.
In atopic dermatitis, phototherapy is widely used as a useful adjunct to medical treatment. This allows not only to improve symptoms, but also to reduce the use of steroid drugs. Other physiotherapeutic methods are also used (lazarotherapy, ultraphonophoresis, alternating magnetic field, EHF-therapy.
Health resort treatment can have a good effect.
The possibility of treating atopic dermatitis with anti-IgE antibodies (omalizumab, or Xolair) is being considered. A similar method began to be used in moderate and severe bronchial asthma. Research on its use in atopic dermatitis has not yet been completed.
Another drugs used in atopic dermatitis: Sunamol C (from eggshell), zodak, smear the rash to choose from and according to the situation, either elocol (if itching is very strong) or drapolene. Ointment Fucidin G and drops Fenistil, Creon, Zyrtec.
Prevention of atopic dermatitis.
Atopic dermatitis is one of the most common skin diseases in childhood, occurring primarily in children with a hereditary predisposition to allergic diseases, having a chronic relapsing course, age-related features of the localization and morphology of inflammation foci, and due to hypersensitivity to allergens.
Hereditary burden for atopy is estimated at 50-70% or more. It was revealed that in such children one of the parents suffers from allergies in 20-50% of cases. When both parents suffer from allergies, the likelihood of developing atopic dermatitis in a child increases to 75%. In addition, it has been proven that 80% of patients with atopic dermatitis also have a hereditary burden for such atopic diseases as atopic bronchial asthma, atopic conjunctivitis, urticaria, vasomotor rhinitis.
Atopic dermatitis affects girls to a greater extent (66%), less often boys (35%). According to many studies, atopic dermatitis is more common in children living in megacities than in children living in rural areas.
Measures to prevent atopic dermatitis should be carried out even before the birth of a child - in the antenatal period (antenatal prophylaxis) and continue in the first year of life (postnatal prophylaxis).
Antenatal prophylaxis should be carried out together with the allergist, doctors of the gynecological department and the children's clinic. Significantly increase the risk of atopic dermatitis formation by massive drug therapy of a pregnant woman, exposure to occupational allergens, unilateral carbohydrate nutrition, abuse of obligate food allergens, etc.
In the early postnatal period, it is necessary to try to avoid excessive drug treatment, early artificial feeding, which lead to stimulation of the synthesis of immunoglobulin. A strict diet applies not only to the child, but also to the breastfeeding mother. If there is a risk factor for atopic dermatitis, proper skin care of the newborn, normalization of the gastrointestinal tract is necessary.
But it is not worth completely excluding contact with allergens, it is necessary, as it were, to gradually accustom the child's body to them and, without exacerbation of atopic dermatitis, in minimal quantities, one by one, introduce such products into the baby's menu.
The article was written using the literature: Atopic dermatitis in children: diagnosis, treatment and prevention.
Scientific and practical program of the Union of Pediatricians of Russia. M., 2000
Dermatitis occurs in children as a consequence of the increased sensitivity of the child's body to external or internal stimuli. Dermatitis is an inflammation of the skin. For timely and correct treatment of dermatitis, it is necessary to determine what type it belongs to.
Causes of the development of dermatitis in a child
The development of dermatitis in a child indicates his congenital or acquired predisposition to allergies. Most often, the disease occurs in infants and children under 4 years of age, then cases of the development of the disease are less and less common.
Risk groups for developing dermatitis:
- numerous infectious diseases during pregnancy and after the birth of a child;
- the tendency of one or both parents to allergies;
- long-term medication during pregnancy and after the birth of a child;
- complicated pregnancy and childbirth;
- improperly organized feeding;
- constant exposure to exhaust gases, smoke, dyes and other pollutants;
- non-observance of hygiene rules.
Remember! Children are very susceptible to any influences on the body, especially for children of the first year in life, who are just learning to live and interact with all manifestations of the world around them.

Symptoms
Types of dermatitis have similar symptoms that make it difficult to identify a specific type.
How it manifests itself:
- lack of appetite, capriciousness, poor sleep;
- rashes, cracks, crusts form;
- there is itching, redness, swelling of the skin;
- temperature increase.
The severe course of the disease may be accompanied by wheezing, swelling on the face.
Important! If a complicated case of dermatitis is detected, the child needs urgent hospitalization. Lack of timely assistance can lead to respiratory arrest, anaphylactic shock, convulsions.
The first symptoms of the disease should be a signal for parents to visit a doctor. He will collect an anamnesis, prescribe laboratory blood tests for allergens. In children older than 3 years, the allergen is detected by skin tests.

Atopic dermatitis
- Clothing made from natural fabrics. Pay special attention to washing powders and other household chemicals, often the allergen is contained in them.
- Antihistamines: Suprastin, Tavegil, Claritin.
- Ointments and creams to moisturize the skin, relieve inflammation.
- Compliance with the rules of personal hygiene.
- When breastfeeding, a special diet for mom. Kids have porridge, vegetable purees on the menu.
Interesting to know! There is a treatment technique based on the introduction of doses of the allergen into the body in order to increase its resistance over time. Starting with small doses, the body is allowed to get used to the allergen.

The best way to moisturize the skin is. Fatty products contained in cosmetics are called emollients. They contribute to the easy distribution of the cream over the skin, do not allow moisture to evaporate from the surface of the skin.
The most common and available emollients:
- Mustella Stelatopia;
- Emolium;
- Topicrem;
- Locobase;
- La Roche Pose Lipikar.
The main mistake of parents is to stop applying the cream to the child's body when the disease is in the calm stage.

Seborrheic dermatitis
Seborrheic dermatitis usually affects the scalp of a child, it can appear in the sternum, on the legs, in the groin, in the axillary folds of the skin, on the eyebrows and eyelids. The causative agent of the disease is a fungus, and the main manifestation of the disease is yellow crusts on the skin (gneiss). The disease can occur due to nervous stress, malnutrition, hormonal imbalance.
- daily water procedures;
- use of therapeutic shampoos: Nizoral, Kelual DS;
- therapeutic creams: Bioderma, Saforel, Friderm.
The duration of treatment and drugs are prescribed by the attending physician.
Important! Do not panic, seborrheic dermatitis in infants usually manifests itself at 2-3 weeks of age and disappears by the end of the second month.

Diaper dermatitis
Rashes occur due to non-compliance with the rules of hygiene and care for delicate baby skin. Prolonged contact with urine and feces, untimely diaper change lead to inflammation. Less commonly, diaper dermatitis is caused by a reaction to a certain brand of diapers, soap, shampoo, or baby laundry detergent due to the allergens they contain.
How it manifests itself:
- rash on the buttocks, genitals, inner thighs;
- skin redness;
- pain, itching, provoking crying, refusal to eat, irritability.
It consists of the following:
- Strict adherence to hygiene measures.
- Choose a suitable diaper for your baby, change it every 4-6 hours. If the child poops - change immediately, do not keep in a dirty diaper.
- Use hypoallergenic shampoos and soaps.
- More often arrange air baths.
- Use powder, apply it to dry and clean skin.
- , D-Panthenol are excellent for the treatment and prevention of diaper dermatitis.
Lack of timely treatment can lead to the formation of pustules with an unpleasant odor, erosion.
Allergic dermatitis
Allergic dermatitis occurs due to the imperfection of the liver in children, it does not cope with its work (detoxification of substances), the immune system is weakened, the body reacts with the allergen.
Allergen entry into the child's body:
- with food, with mother's milk;
- skin contact;
- through the respiratory tract.
Treatment should begin with the exclusion of the allergen from the diet or direct contact with the baby's skin. Compliance with a diet that excludes all potentially allergenic foods: chocolate, nuts, seafood, citrus fruits, etc. The doctor may prescribe antihistamines, enterosorbents to accelerate the removal of substances from the body, ointments to moisturize and relieve inflammation from the skin.
Remember! Often children with age simply "outgrow" such an allergy. As you grow, your body's resistance increases.

Weeping dermatitis
Weeping dermatitis is skin inflammation characterized by the appearance of cracks with the separation of pus or ichor from them.
Reasons for the development of the disease:
- food allergy;
- reaction to medications;
- diseases of the gastrointestinal tract;
- reaction to external stimuli: cosmetics, household chemicals, etc.;
- disorders of the nervous system.
In children, the face, flexion/extension zones of the joints are usually affected.
Attention! To treat the disease, it is necessary to conduct a thorough diagnosis in order to determine the cause of its occurrence. The doctor prescribes treatment based on the tests and examinations.
Irritation on the skin appears under the influence of direct sunlight. With this type of disease, even a short exposure to the sun causes redness, itching, swelling, and a rash.
The reason for its occurrence is not the sun's rays themselves, but the substances contained in the skin of the child, and reacting with ultraviolet (histamine, acetylcholine). Most often, such a reaction is caused by diseases of the liver or intestines, endocrine disorders, beriberi, perfumes, cosmetics, creams, plant pollen that has got on the skin, and taking medications.
Treatment consists of taking antihistamines. To relieve itching, zinc ointment or non-hormonal drugs are used: Elidel, Fenistil-gel. Perfectly relieve itching and irritation baths with herbs (string, chamomile, sage).
To prevent the occurrence of solar dermatitis, you should try to avoid being in the sun at the most aggressive time (from 11 a.m. to 5 p.m.), apply sunscreen on the child’s body, and the diet should not include fatty, salty, fried, allergenic foods.

Perioral dermatitis
An inflammatory condition of the skin around the mouth is called perioral dermatitis. Small pimples (papules, vesicles, pustules) form around the mouth. It can occur due to climate change, weakening of the immune defense, disruption of the digestive tract, stress, hormonal imbalance, cosmetics.
For treatment, the principle of zero therapy is applied. It consists in the abolition of all used ointments, creams, cosmetics, especially glucocorticoid drugs, and a decrease in contact with water. Antihistamines are prescribed: Suprastin, Tavegil. Elidel cream, Metronidazole, Erythromycin, tetracycline ointment.
Remember! It is necessary to avoid sun exposure, stop the use of cosmetics.
Dermatitis of any type is an unpleasant disease, and sometimes very dangerous, if not properly treated. At the first signs of the disease, you should immediately consult a doctor.
Contact dermatitis is an inflammation of the skin that occurs when an allergic substance comes into contact with them.

Seborrheic dermatitis is a skin disease caused by overactive sebaceous glands. This state is easy
Content
A disease in which local redness, rash and inflammation of the skin occurs is called dermatitis. The disease manifests itself in a person at any age. Dermatitis in children is usually the result of an infection, a toxic effect on the skin, or a symptom that indicates an allergy. In order to choose the right medicine, it is necessary to identify the cause of the disease.
What is dermatitis
This is a disease of the skin that is caused by biological, chemical, physical or internal agents. In children, pathology develops mainly against the background of a hereditary tendency to allergic reactions. Often, skin inflammation in infants occurs in the first months of life. What is dermatitis in children after 4 years, mothers know much less often. The following groups are at risk:
- children in whom both parents suffer from any form of allergy;
- frequent infectious diseases of the mother during pregnancy;
- improper feeding;
- long stay in a highly polluted environment (exhaust fumes, dyes, smoke).
Classification of dermatitis
Groups of skin diseases have a complex classification. Types of dermatitis and the names of subspecies depend on the following factors:
- the reaction of the body to the action of the pathogen: inflammatory, infectious, allergic, fungal;
- method of pathogen application: orthopedic, retinoid, contact, atrophic;
- the nature of the course of the disease: chronic, acute, subacute;
- rash size: nodular, nummular, miliary;
- names according to primary symptoms: scaly, vesicular, bullous;
- leading symptoms of a dermatological disease: itchy, exudative, dyshidrotic.
allergic
This type of skin disease is chronic. Allergic children's dermatitis is a term that refers to a whole group of pathologies that develop against the background of an allergy that occurs due to a particular irritant. This is not a skin disease, but a sign of disorders in the immune system. Also, allergic dermatitis in children develops against the background of insufficiency of the functions of the liver and digestive system.
A baby, just born, is attacked by many microbes, which the body learns to resist only gradually. The process of producing antibodies does not start immediately, so the immune system does not adequately respond to allergens, provoking inflammation of the dermis. For this reason, infants are more likely to develop various kinds of allergies.
Allergic dermatitis in children symptoms
Allergodermatitis manifests itself in each age category in different ways. The largest group is the period from birth to 2 years. Skin manifestations look like dry or weeping hyperemic areas that are localized on the folds of the limbs and face. Often, the symptoms spread to the trunk and scalp. What allergic dermatitis looks like in older children and adolescents:
- rashes on the knees, elbows, décolleté, abdomen, neck, buttocks and even the external genitalia;
- swelling, redness of the epidermis with crusts and plaques;
- severe itching, scratching;
- when an infection occurs, pustules, weeping occur.
atopic
Neurodermatitis (dermatitis) is an extremely common disease in pediatric practice. Not all mothers know that atopic dermatitis is an ordinary diathesis, which has a more pronounced form. The term "atopy" is taken from the Greek word for "alien", which is associated with the ingestion of an allergen into the body. Its main difference from an allergic disease is expressed in the conditions of occurrence and mechanisms of action. Treatment of atopic dermatitis in children is more difficult, since it is characterized by a genetic predisposition.
Atopic dermatitis symptoms
Like allergic dermatitis, atopic dermatitis also resolves differently, depending on age. The clinical picture is varied and is determined by the severity and duration of the disease. Almost always, this type of inflammation is accompanied by severe itching, small peeling and a rash on any part of the skin. Against this background, the child becomes aggressive, excited. As a result of prolonged scratching, thickening of the skin layers occurs.
Causes of atopic dermatitis in children
To know how to treat atopic dermatitis in a child, you first need to identify the cause of its occurrence. The disease manifests itself against the background of a combination of adverse environmental factors and genetic disposition. Atopic dermatitis causes:
- food allergy;
- severe pregnancy;
- gastritis;
- intestinal dysbacteriosis;
- enterocolitis;
- helminthic invasion;
- household allergens - pollen, mites, washing powders.
contact
The disease is characterized by skin lesions in those areas that are in direct contact with the irritant. Contact dermatitis in a child can develop seasonally, especially often its manifestations are observed in winter. The disease goes through several stages:
- at first, only redness and swelling (erythremal form) is observed on the skin of the child;
- then abscesses and sores are added (vesicular-painful stage);
- scabs form at the site of ulcers, leaving behind scars (necrotic stage).
The causes of the inflammatory reaction of the epidermis can be low or high temperatures, exposure to ultraviolet radiation, increased skin sensitivity. Often, the disease is provoked by cosmetics, synthetic clothing, diapers or household chemicals. Insect bites or flowering plants may be involved in the appearance of this type of disease. Gold jewelry and other metals also sometimes provoke an allergic reaction on the child's body.

infectious
This disease indicates an infection that has appeared in the body. The viral form of skin lesions is not so much an independent pathology as a symptomatic factor of other diseases. Infectious dermatitis in children can occur after chickenpox, rubella, measles, or scarlet fever. Sometimes it manifests itself after surgical interventions and getting into open wounds of staphylococci, streptococci or other pyogenic microorganisms. Skin reactions appear depending on the symptoms of the primary disease:
- with measles - a papular rash;
- with scarlet fever - red spots that merge with each other, forming extensive areas of damage;
- with chickenpox - subtle redness, eventually turning into small blisters with transparent contents;
- with typhus - self-opening vesicles, in place of which a crust forms.
seborrheic
A variation of this skin inflammation affects the scalp, cheeks, nose, eyebrows, ears, chest, and back. In a mild form, seborrheic dermatitis manifests itself in the form of small flaking scales and dandruff. A severe form of the pathological process looks like foci of inflammation in the form of round or oval spots covered with a continuous crust. The danger of the disease is that it is extremely difficult to get rid of it, especially at a later stage, when the affected areas become infected and pus appears in them.
The causative agent of seborrhea are the fungi Malassezia furfur, which are introduced into the skin and provoke gneiss (yellowish-gray crusts). Microorganisms are conditionally pathogenic, which means that they will live there permanently. As soon as favorable conditions occur, the fungi become active and cause undesirable changes on the skin. Factors that trigger the mechanism of microbial reproduction:
- Internal. These include diseases of the nervous system, stressful situations, suppression of the immune system.
- External. These include: the adverse effects of poor ecology; washing the body and hair with products containing alkaline substances; profuse sweating, hereditary predisposition.
fungal
The disease is often latent in nature, so it is difficult to diagnose. Fungal dermatitis occurs in both acute and chronic forms. If it is not cured at the initial stage, then there is a high probability of infection of family members. The symptomatology of the disease is similar to other skin pathologies - it is an allergic rash, accompanied by a burning sensation, severe itching. If left untreated, fungal eczema occurs on the legs and feet.
The main cause of fungal infections of the skin is infection of the mucous or open areas of the body with pathogenic bacteria. Often this happens through contact with an already infected person, but there may be other reasons:
- taking medications;
- pathology of the gums or teeth;
- gastrointestinal problems;
- genetic features;
- diseases of the urinary system;
- immunodeficiency.
Oral
It is characterized by papular-spotted rashes in the chin and perioral cavity. Oral dermatitis in a child and an adult has the same clinical picture. In adolescence, the disease occurs more often, due to changes in hormonal levels and lack of vitamins in a rapidly growing body. In infants, pathology can occur due to weathering of the skin in the cold or due to dysbacteriosis. The rash clinic is bright, specific, having certain characteristics:
- Localization. The rash occurs symmetrically around the chin and mouth. There is a white stripe of intact skin between the area of the rash.
- Prevalence. Pimples can go to the nasolabial triangle and the corners of the lips.
- Quantity. First, there are single papules. As the pathology develops, they are grouped into conglomerates.
- Color, diameter. Papules are localized on red spots, but have a white color. Diameter - up to 3 mm.
- Associated manifestations. With improper therapy, pustules, weeping, irritation may occur. With too intensive treatment, the inflammatory process can worsen.

Dry
This type of disease is a consequence of the low content of lipids in skin cells. Often, dry dermatitis develops against the background of atopic or seborrheic, when the stratum corneum of the epidermis contains an insufficient amount of ceramides. Among the common causes of illness, doctors distinguish:
- frost or drought;
- internal diseases of the body;
- heredity;
- psychosomatic factors;
- household irritants;
- insufficient humidity in the room;
- long-term drug treatment;
- improper diet of the mother during lactation.
Treatment of dermatitis in children
It is much easier to cure dermatitis in an infant than in adolescent girls and boys. The well-known pediatrician Komarovsky claims that at the first signs of the disease, parents need to contact an experienced pediatrician to establish the correct diagnosis. To cure the pathology, it is necessary to strictly follow all the doctor's instructions. Particular attention should be paid to the nutrition of the baby - look at the body's reaction to the adoption of any food, especially new ones.
Drug treatment of dermatitis in children includes the appointment of tablets, creams, ointments, syrups. All drugs of external and internal action are divided into categories:
- glucocostosteroids, which reduce inflammation, reduce itching;
- antihistamines, relieving allergic manifestations;
- antiseptic, helping to destroy germs;
- immunostimulating, which strengthen the immune system;
- dexpanthenol, used to treat skin at any stage.
Prevention of dermatitis
After diagnosing skin inflammation, it is important to eliminate the cause of the disease. For example, atopic dermatitis, the prevention of which lies in the diet, can be removed if the allergen that provoked the disease is excluded. If the pathology has arisen in a formula-fed infant, then the main preventive measures are enhanced hygiene and revision of milk formulas.
With seborrhea, it is necessary to exclude cosmetics that arouse suspicion - it is better to do them yourself at home from folk remedies. In addition, it is necessary to regularly smear the scalp with a preparation recommended by the pediatrician. With an exacerbation of seborrhea, polydermatitis or other types of skin inflammation, it is necessary to put the child on a special diet that excludes canned food, smoked meats, bee products, nuts, seasonings, citrus fruits, cocoa and some berries from the daily menu.
Dermatitis in children is referred to as inflammatory skin processes that appear under the influence of various irritants on a sensitive children's body. Many attribute diathesis, common among children, to atopic dermatitis. Actually this is not true. Such manifestations on the skin only indicate the child's tendency to allergic manifestations, and only in 10% of cases diathesis is a symptom of dermatitis.
This disease is quite common in children under one year old. The well-known rash on the baby's bottom is also one of the types of dermatitis. This is due to intense changes in the body of the child after his birth. They affect almost all organs and systems, including the immune system. Over time, the child's immunity is restored, but during the period of formation and improvement of the body, children are exposed to various irritants. In the treatment of dermatitis, various means are used depending on the causes and types of the disease.
What causes dermatitis in children
"Dermatitis in children is an inflammatory skin reaction due to hypersensitivity to external stimuli." The development of the disease in a child is associated with a genetic predisposition to allergies. Less commonly, it is an acquired feature of the body. As a rule, such dermatitis in children appears in the first months of life (diaper dermatitis on the pope, seborrheic crusts, diathesis, etc.), and after 4 years of age they are relatively rare.
The following categories of children are at increased risk of dermatitis:
- whose parents (one of the parents) suffer from a food or other type of allergy;
- children whose mothers suffered infectious diseases during pregnancy;
- babies who had viral diseases in infancy;
- born to women who had complications during pregnancy or childbirth;
- children whose mothers often took medications during pregnancy;
- children who were fed with unadapted infant formula, ahead of time, as well as highly allergenic foods;
- children constantly living in an environment polluted with harmful substances;
- babies raised in an environment where basic hygiene rules are not respected.
These are the common causes of this disease. Each individual species has its own causes and symptoms, which in turn affects the treatment.

The main types of dermatitis in children and their symptoms
- Seborrheic dermatitis. This type of disease in question develops mainly on the head of the child and is very rarely localized to other parts of the body. The main symptom is the appearance of greasy yellowish crusts on the scalp. Less commonly, the disease develops in the ears, neck, chest, groin (groin folds). It is characteristic that itching is absent or not pronounced. Seborrheic crusts do not occur on the arms, legs, buttocks and other parts of the body. If such rashes are present on the body, excluding the scalp, consult a dermatologist for a diagnosis.
The cause of the disease is a fungus of the genus Malassezia furfur. It is he who is "responsible" for the presence of symptoms of seborrheic dermatitis and in its treatment, if necessary, means are used that are aimed at combating this fungus.
This type of skin disease develops in children of two to three weeks of age on the scalp. If proper treatment is not carried out, it is possible to attach a secondary bacterial infection. This subsequently greatly complicates the diagnosis and course of the disease.
- Atopic dermatitis. This type of dermatitis is characterized by inflammation of the skin. Symptoms that distinguish it from similar types of dermatitis are redness of the skin and its dryness, peeling, and the appearance of watery blisters. The rash is characterized by intense itching. It most often occurs on the face and hands, less often on other parts of the body.
The main reason why dermatitis develops is the genetic predisposition of the baby. With a more detailed study in the blood test, an increased level of antibodies is observed, which are responsible for the appearance of allergic reactions. These indicators indicate that the slightest pathogen can cause allergies. Allergens can enter the body in three ways: through the respiratory system (respiratory allergy), through skin contact (contact), with food and drink (causing food allergies).
Often, in children prone to atopic dermatitis, along with other symptoms, there is a disorder in the gastrointestinal tract (dysbacteriosis). It appears in babies up to 6 months of age. However, there are cases when the disease is observed in preschoolers and adolescents. At the same time, the symptoms of the disease in children of different ages are different.
The main symptoms in children under 2 years of age:
- red rashes on the face and neck, on the arms in the area of the elbow joints, groin;
- the presence of small watery bubbles;
- the appearance of small cracks in the skin;
- the presence of small crusts that have a yellowish color;
- dry skin, which is accompanied by peeling;
- pronounced itching of areas affected by dermatitis;
Symptoms of atopic dermatitis in preschool children:
- inflammations are localized mainly in the skin folds, there are frequent cases of rashes on the hands (palms) and legs in the area of the feet;
- the course of the disease acquires a chronic form, characterized by acute periods and remissions;
- thickening and dryness of inflamed areas of the skin or the presence of rashes in the form of watery vesicles;
- sleep disorder associated with constant severe itching.
- Diaper dermatitis. This skin disease is known to most parents. Diaper dermatitis is an inflammatory disease of the skin in the thighs, genitals and buttocks, which is caused by prolonged contact with the feces of a child.

The reasons why dermatitis develops in children are due to the following factors:
- non-compliance with the rules of personal hygiene of the baby (rare washing and bathing);
- non-compliance with hygiene procedures by the mother (changing a diaper with dirty hands);
- incorrectly sized disposable diapers (the use of diapers of the wrong size rubs the delicate skin of the child, which leads to the development of inflammation);
- allergy to washing powder and products used in baby skin care, improperly selected soap;
- intestinal dysbacteriosis;
- having a food allergy.
The main symptoms of diaper dermatitis:
- small rashes in the perineum and redness of these skin areas;
- increased sensitivity of damaged areas of the skin when touched;
- severe itching;
- restlessness and irritability of the child;
- causeless crying;
- restless sleep;
- the appearance of pustules and an unpleasant odor (a sign of a secondary infection).
Diaper dermatitis develops exclusively in the area of contact with the diaper: in the groin, on the pope, legs (inner thighs). If this kind of rash is found on the head, behind the ears, on the arms, legs and other parts of the body, then this is a completely different type of skin disease that a pediatrician, dermatologist or allergist can diagnose.
- Candida dermatitis. This disease is a type of diaper dermatitis, and its name is due to the fungus of the genus Candida albicans, which causes dermatitis. Note that inflammatory skin diseases can occur even with careful observance of the requirements of the child's personal hygiene.
Candidal diaper dermatitis is characterized by a bright red, painful rash with patchy edges. Lesions are located in the groin (groin folds) and may be dry or weepy.
- Contact dermatitis in children
The name of the disease speaks for itself. It is a type of allergic dermatitis and occurs with constant contact of the irritant with the skin of the child. Most often it manifests itself in the area of constant friction of clothes (on the arms and legs), rough seams, the use of a cream that irritates the child's skin.
The main symptoms of the disease is a symmetrical arrangement of reddish rashes, accompanied by itching. Sometimes rashes appear in the form of bubbles with liquid, which, opening up, leave weeping wounds. The affected areas are characterized by swelling of the skin.
With untimely treatment and elimination of the cause that causes dermatitis in children, the disease becomes chronic. Therefore, it is very important to contact a specialist in time to identify the irritant and avoid repeated contact with it.
- Viral dermatitis. This type of dermatitis is one of the symptoms of an infectious disease or its consequence. The most pronounced infectious dermatitis in scarlet fever, chicken pox, typhoid fever and measles. It can appear on any part of the body, incl. on the arms and legs and even on the pope.

Traditional treatment of childhood dermatitis
How to cure dermatitis in a child? This question is asked by parents whose children have this disease. There are two ways to go: the traditional way or using traditional medicine. Whatever treatment you choose, remember that only a doctor, after a thorough examination and identification of the cause of dermatitis, can prescribe adequate treatment that will not harm the child and help get rid of the disease.
Treatment depends on the diagnosed type of dermatitis.
The basis of the treatment of seborrheic dermatitis is daily shampooing, using special products, after which the crusts are removed mechanically using a comb with soft bristles. As a rule, in infants up to two months of age, seborrhea goes away on its own and does not require special treatment. Occasionally, pediatricians recommend the use of shampoos that relieve inflammation, thereby reducing the formation of gneiss (crusts). To facilitate the removal of crusts, you can use special oils and emulsions. The need to use medicated shampoos (Nizoral, Kaleual) and topical medicines (Saforel, Bioderma, Friederm Zinc) and the duration of the course are determined by the pediatrician.
In order to begin the treatment of atopic dermatitis, it is necessary to make sure that the cause of the rash is an allergy and to exclude other infectious and other skin diseases. To do this, you should contact a pediatrician, who, in turn, can refer you to narrow specialists (dermatologist, allergist) to confirm the diagnosis.
Young patients diagnosed with atopic dermatitis, incl. and contact dermatitis in children, it is recommended to adhere to a special diet that excludes allergens. This is especially true for children who suffer from food allergies, which manifest themselves mainly on the face and hands. The main drugs that are prescribed for children are topical glucocorticosteroids (Afloderm, Advantan) and antiallergic drugs. Most pediatricians prefer drugs that do not contain hormones. They do not cause serious side effects. These drugs include Elidel ointment, which is safe for children's health.
The treatment regimen is individual in each case. Based on the symptoms of the disease, a pediatrician, dermatologist or allergist selects the most effective methods of therapy.
Treatment of diaper dermatitis involves frequent change of disposable diapers (at least every 4 hours) and personal hygiene of the child. In some cases, pediatricians strongly recommend abandoning disposable diapers until the symptoms of the disease on the buttocks, thighs and genitals of the child completely disappear. Air baths are very useful for the baby and have a positive effect on wound healing. After performing hygiene procedures, the baby's skin must be well dried and a moisturizing cream, ointment or emulsion (D-Panthenol, Bepanten) applied.
Candidiasis diaper dermatitis in children is treated mainly with antifungal drugs. These include azoles (Clotrimazole, Nizoral, Travogen), allylamines, antibiotics that eliminate the fungus (Pimafucin, Nystatin). These drugs are used externally.. In some cases, drugs are prescribed in tablets.
Viral dermatitis involves the treatment of the disease itself, which causes inflammatory reactions in the hands and feet. To alleviate the condition of the child, antihistamines and antiallergic drugs that relieve itching are used.
Folk remedies in combination with the main treatment also have their advantages and disadvantages. Despite all the seeming safety, some tinctures and decoctions can aggravate certain types of dermatitis in children. It is possible to use certain herbs and fees without fear for the health of the child only after consulting with the attending physician.
How to prevent dermatitis in children
An excellent preventive measure for dermatitis in children is prolonged breastfeeding, while the mother observes the correct diet. In addition, limit the use of hygiene products (soaps, creams). With age, the child's tendency to allergies and dermatitis disappears. Almost all types of dermatitis are treatable. Do not forget that it is much easier to prevent children's dermatitis than to treat it! If you notice the slightest changes in the skin on the arms, legs, back, head, butt of the child or on other parts of the body, do not postpone a visit to the doctor.
Auth. Gavrilenko Yu.