Screwing in diabetes: causes and ways to fight. False acute belly in patients with diabetes mellitus, severe abdominal pain and diabetes
Disorders of the gastrointestinal tract (gastrointestinal tract) are common among all people, including patients. At some point in the life of the patient with diabetes, the possibility that he will have a problem with the gastrointestinal tract, be it ulceratively, stones in a busty bubble, an irritable colon syndrome, food poisoning or other disease, extremely high.
More than 75% of patients with diabetes are reported on the essential signs of the gastrointestinal disorder. The entire gastrointestinal tract may be affected, from the oral cavity and esophagus to the colon and anorectal area. Thus, the complex of signs that patients experience can vary significantly. Frequent complaints may include dysfagia, early saturation, reflux (reverse outflow), constipation, abdominal pain, nausea, vomiting and diarrhea.
And the acute and chronic can lead to certain complications of the gastrointestinal tract. Diabetes is a systemic disease that can affect a lot of organism organs, and the gastrointestinal tract is no exception. As with other complications of diabetes, prolonged mess in diabetes compensation and bad glycemic control are associated with more serious problems of the gastrointestinal tract.
Most complications of Diabetic gastrointestants in diabetics are associated with the dysfunction of neurons transmitting the signal to the enteral nervous system. Just like the nerves in the legs can be damaged by peripheral neuropathy, the defeat of the nerves of the intestine can lead to abdominal neuropathy. This is the type of autonomous neuropathy can lead to deviations in intestinal mobility, sensations, secretion and absorption. Various nerve fibers can or stimulate or prohibit the mobility and functionality of the intestine, and damaged nerves, can lead to slowing down or accelerating the intestinal function.
Esophagus and stomach during diabetes
Diabetic gastroparesis - Condition in which the release from stomach is delayed, leading to the detention of the contents of the stomach. It can cause inflating, stretching, abdominal pain, nausea or vomiting. Stagnation of the stomach can lead to a deterioration of gastroesophageal reflux along with signs of heartburn and mechanical joking the contents of the stomach. In addition, fatty foods and very fibrous products usually slowly come out of the stomach and can be poorly tolerated.
 Diagnosis Gastroparesis is often assumed based on only symptoms. The top endoscopy of the gastrointestinal tract is useful to exclude the obstruction of the stomach or duodenum, but does not provide an accurate physiological assessment of the liberation of the stomach. Radiography with the Barium of the Top Departments of the GST can confirm the delayed liberation of the stomach. However, the top row of the gastrointestinal tract usually undiagnose, since liquids can be released from the stomach. Despite severe deviations in the ability to release solid stomach materials in the duodenum.
Diagnosis Gastroparesis is often assumed based on only symptoms. The top endoscopy of the gastrointestinal tract is useful to exclude the obstruction of the stomach or duodenum, but does not provide an accurate physiological assessment of the liberation of the stomach. Radiography with the Barium of the Top Departments of the GST can confirm the delayed liberation of the stomach. However, the top row of the gastrointestinal tract usually undiagnose, since liquids can be released from the stomach. Despite severe deviations in the ability to release solid stomach materials in the duodenum.
Surveys of nuclear medicine liberation of the stomach is the best confirming test for gastroprota assessment. Test solid food is griming with food containing isotope technetium, swallows, and scintigraphy is used to quantify the rate of release of the stomach. This test is highly sensitive and specific, despite positive parties, there may be negative in response to drugs that speed up or slow the pace of the liberation of the stomach. Performing diagnostics, it is better to measure the indicators of the liberation of the stomach, when patients do not take medicines that can affect the rate of liberation of the stomach.
Some types of treatment may bring benefit in the management of diabetic gastroparesis. Consumption of often small food portions can give some symptomatic relief. It can also be advantageous to exclude products with a high content of fats and high fibers. It is recommended to "sit" on a liquid diet during the enhancement of a gastroprota. If signs deteriorate, parenteral hydration and nutrition may be required. A nasogastric probe can also be used during serious cases.
Numerous medicines, as shown, provided some advantage in the treatment of gastroprota. Raglan is a dopaminergic antagonist who increases the liberation of the stomach and has anti-luxurious properties. Unfortunately, it crosses the hematostephalic barrier and causes frequent neurological side effects, such as drowsiness, dyskinesia body muscles, dizziness, diarrhea that takes place after the drug is stopped.
Cispride (Prepulsid) is a prokinetic substance that is very effective in facilitating the release of the stomach. A pharmacological problem common with the regulated does not occur with cisapprid, and the tolerability of the drug is excellent.
Domperidon (Motilium) is another prokinetic remedy, similar to the regulated, which speeds up the liberation of the stomach, but does not cross the hematostephalic barrier and has very few side effects.
Eritomicin has unique properties that stimulate the mobility of the stomach and may be favorable for some people. This medicine stimulates the stomach motor. Unfortunately, eritomycin has many potential side effects including nausea and can be intolerable.
You can still bring a lot and describe medicines from gastroprota, but it is better to consult a doctor ,. The article shows what complications of the gastrointestinal tract from diabetes, and how to identify them.
Recently, a new approach to the immune gastroporasis appeared, an implanted stomach pacemaker is used. It has long been recognized that many patients with gastroparesis have the wrong electric rhythms of the stomach. Surgical accommodation of a stomach cardiovel conducted in the department gastroenterology in Israel As shown, accelerated the liberation of the stomach and ensured the symptomatic relief in patients.
Throw smoking, make up easy exercises after meals (for example, walking), and dietary manipulation (multiple meals with small portions and caring from high fiber and oily food) can also improve the release of the stomach. What is most importantly attentive attitude to blood glucose control can have a huge impact on gastroparesis.
Ulcerative disease
- The problem of people and with diabetes without it, affects up to 10% of the population. Acid irritation of the stomach or esophagus leads to heartburn, disorder of the stomach and digestion.
 Helicobacter Pylori, bacteria responsible for most duodenal ulcers and stomach ulcers, it is no more common in patients with diabetes than in the population as a whole. In fact, diabetes itself does not increase the risk of developing ulcers. People with ulcers and similar ulcers are attributed to the same way regardless of whether they have diabetes.
Helicobacter Pylori, bacteria responsible for most duodenal ulcers and stomach ulcers, it is no more common in patients with diabetes than in the population as a whole. In fact, diabetes itself does not increase the risk of developing ulcers. People with ulcers and similar ulcers are attributed to the same way regardless of whether they have diabetes.
The treatment is to suppress the secretion of the acid of the gastric juice with antisecretory drugs (H2-receptor antagonist or proton inhibitors of the pump). If the chielicobacter pylori is present, then bacteria will be treated with a certain antibiotic regime along with antisectory substances. General antibiotic modes include 2-week Amoxacillin (Amoxyl) / Clarithromycin (Biaxin), Metronidazole (Flagyl) / Clarithromycin, Metronidazole / AMOXACILLIN.
Candidiasis
Patients with diabetes may be sick of candidides in the gastrointestinal tract, especially when control over blood sugars was bad. Candidiasis in the mouth (candidal stomatitis) is characterized by a thick white coating of the tongue and the throat along with pain and burning disease. If the infection extends further, the result of candidiasis of the esophagus, it can cause intestinal bleeding, heartburn and difficulties with swallowing.
Candidiasis of the oral cavity can easily be diagnosed with physical expertise, but Ezophagitis of the candidiasis requires endoscopy for an accurate diagnosis. Very effective treatment is required, focused on the destruction of candidosis with antifungal drugs, such as nastatin (microstatin), ketoconazole (nipped) or fluconazole (dieflux).
In some cases, prolonged diabetes, the abdominal nerves of the small intestine, can be affected by leading to incorrect motor skills, secretion or digestion. This leads to signs, such as abdominal pain, inflating and diarrhea. The delayed liberation and stagnation of liquids in the small intestine can lead to an excessive growth syndrome microflora leading to diarrhea and abdominal pain.
Metoklopramide and cisaprid can help speed up the passage of liquids through the small intestine, while the antibiotics of a wide range of action will reduce bacterial levels.
 Diagnosis to put can be quite difficult and may be required by the intubation of the small intestine for. The hydrogen respiratory test may be useful in diagnosing over-increasing microflora growth. All these tests are somewhat severe, but are often an effective means of diagnosing and treating this disease.
Diagnosis to put can be quite difficult and may be required by the intubation of the small intestine for. The hydrogen respiratory test may be useful in diagnosing over-increasing microflora growth. All these tests are somewhat severe, but are often an effective means of diagnosing and treating this disease.
Most antibiotic modes, as shown, were effective, including 5 to 10-day tetracycline courses, ciprofloxacin, amoxicillin, or tetracycline. A short course can provide extensive relief, but as a rule, additional antibiotics courses are required when signs are returned in a few weeks or months.
Over time, abdominal neuropathy can lead to chronic abdominal pain syndrome, similar pain peripheral neuropathy in the legs. This disease is very difficult to treat, but it sometimes responds to painkillers and tricyclic antidepressant drugs, such as amitriptyline (elavil). Unfortunately, this may lead to the dependence of drugs, patients with chronic painful abdominal neuropathy.
Tough intestines for diabetes
Limited information is available regarding the influence of diabetes on the colon. We really know that the abdominal neuropathy can affect the nerves, exciting the colon, leading to a decrease in the intestine of the intestine and the constation. The anatomical deviations of the colon, such as a tumor or diverticulitis, should be excluded with the tubium or colonoscopy.
Supplement of fibers with bran or drug psillium, as well as a high protein diet, increases the water content in feces and can relieve constipation. Moderate laxatives and softeners of the chair will also help. In addition, the cisapride accelerates the colon motorcy and can increase the frequency of detergents.
Diabetic diarrhea
Patients with a long-standing history of diabetes may suffer from frequent diarrhea, and this occurs in 22% of patients. This may be associated with problems in a small intestine or a tolstish intestine. Incorrectly fast passage of liquids can occur in the intestine, leading to an enlarged chair frequency. In addition, deviations in the absorption and processing of the liquid of the colon can develop and lead to an increased volume of the chair, frequency and water content.
Diabetic diarrhea - Syndrome of unexplained non-coming diarrhea in people with a long history of diabetes. This may occur due to autonomous neuropathy, leading to incorrect motorcy and secretion of fluid in the intestine. There are also many intestinal problems that are not rare for people with diabetes, but it can cause diarrhea. The most common is syndrome of irritated colon.
Processing and treatment of diarrhea is the same for patients with or without diabetes. If primary medical analysis diagnosed frequent diarrhea, the treatment is determined to ensure symptomatic care with counter-diarrhea, such as diphenoxylate (lobs) or loperamide (IMODIUM). In addition to consume dietary fibers (bran), Citrucel, metamocil (laxative, increasing the volume of carts) or high fiber products can also compact the consistency of the flowering and reduce the watery diarrhea. In addition, antispasmodic drugs, such as Levzin, Libraks can reduce the frequency of the chair.
 Exocrine pancreatic dysfunction occurs up to 80% of people with, but rarely pronounced enough to lead to any clinical problems with digestion. The pancreas has a huge reserve, and a moderate decrease in the pancreatic secretion of the enzyme rarely leads to difficulties in digestion or absorb carbohydrate, fat or protein.
Exocrine pancreatic dysfunction occurs up to 80% of people with, but rarely pronounced enough to lead to any clinical problems with digestion. The pancreas has a huge reserve, and a moderate decrease in the pancreatic secretion of the enzyme rarely leads to difficulties in digestion or absorb carbohydrate, fat or protein.
Exocrine pancreas may also be affected in some patients with, but to a lesser extent. In people who have secondary diabetes due to severe pancreatitis or surgical removal of the pancreas usually, there are more serious signs of the exocrine lature of the pancreas. Treatment with pancreatic enzyme substitutes (tablets with mesim forte, festal) pancreas is usually effective.
Liver during diabetes
Although the analysis of the liver function is usually incorrect in patients with diabetes, it is unclear whether it is a reflection of obesity, which is so common in patients with type 2 diabetes or whether it is a diabetes effect, which is poorly controlled. Fatic hepatosis of the liver (Non alcoholic steatogeptite) is common in obese people (up to 90%) as well as in people with type 2 diabetes (up to 75%). People with type 1 diabetes with very poor diabetes control can also develop this syndrome, although it is much less common.
 Beep fatty dystrophy can lead to hepatomegaly (liver increase), increasing the hepatic liver and abdominal pain syndrome. Sometimes it can progress to fibrosis and liver cirrhosis.
Beep fatty dystrophy can lead to hepatomegaly (liver increase), increasing the hepatic liver and abdominal pain syndrome. Sometimes it can progress to fibrosis and liver cirrhosis.
The diagnosis is usually put on the basis of clinical indications, but can be confirmed with the ultrasonography of the abdominal cavity and, if necessary, the biopsy of the liver. Metabolic deviations such as gemohromatosis (Pigment cirrhosis) and infectious etiologies, such as viral hepatitis should be excluded by the analyzes.
Therapy is reduced to improving the glycemic control and purpose of a low-calorie diet with low fat content. The calorie restriction will lead to weight loss, will improve glycemic control, to lower serum triglycerides and reduce cholesterol. Ursodol can provide some advantage in the treatment of hepatic seborrhea.
In patients suffering from diabetes, there is an increased morbidity bile stones and problems with the bubble bubble, but they, in many respects, the liver fatty dystrophy are primarily associated with obesity associated with type 2 diabetes, and not to diabetes itself. The obesity leads to the secretion of bile, which is sucked by cholesterol, leading to crystallization and stone formation. Typical symptoms of bile colic include jump-shaking pain in the right upper part of the abdominal cavity, jaundice or pancreatitis.
In the past, patients with diabetes made an operation to remove bile stones because the risk of complications due to stones, such as infection, pancreatitis, or gap bubble gap. However, more recent experience with modern medical service and surgical assistance indicates that it no longer takes place. Thus, patients with diabetes and bile stones need to be treated, similar to patients from diabetes. Surgery is generally recommended only for those people whose bile stones cause clinical signs.
Conclusion
Problems of the gastrointestinal tract in diabetes are common, but in most cases recognized in clinical practice. Duration of diabetes and the degree of control over the glycemic index - the main and severity of the problems of the gastrointestinal tract. The entire treatise may be affected, including the mouth, esophagus, stomach, small intestine, colon, liver and pancreas.
Treatment begins with a complete examination of the patient in the appropriate laboratory, enlighten, and test the gastrointestinal tract. In addition to pharmacological therapy, glycemic control and dietary manipulation play an important role in managing the disorders of the tract in people with diabetes.
Sugar diabetes, being a systemic disease, striking the work of various systems. The development of the autonomous neuropathy provokes the stomach paresis during diabetes mellitus and a number of other trades of the tract, which may affect the entire digestive system or its separate sections. More often, diseases are accompanied by unpleasant symptoms that reduce the quality of life. To avoid such complications, it is necessary to control blood glucose levels.
Communication of diabetes and disease gasts
In 75% of patients with diabetes mellitus, there are violations in the work of the gastrointestinal tract.
Any complications of diabetes have a common cause of development - an increase in blood sugar. This pathology negatively affects the state of nervous tissue and connections between neurons, which is why diabetic neuropathy develops. Diseases of the gastrointestinal tract with diabetes mellitus arise due to disruption of the transfer of nerve impulses in the central nervous system. In fact, the high level of sugar contributes to the development of the abdominal type of autonomous neuropathy.
Autonomous neuropathy is characterized by a violation of the work of the internal organs, in particular, the gastrointestinal tract. Pathology leads to changes in the intestinal peristals in diabetes, violates the normal secretion and suction of the beneficial substances. Nervous endings with a certain effect on them stimulate or inhibit the intestinal motor activity. With the damage to the nervous tissue, the patient has incontinence of feces and a liquid chair or, on the contrary, there are prolonged constipation.
Signs of disorders of the gastrointestinal tract in diabetes
 Constipation or diarrhea can be symptoms of diabetes.
Constipation or diarrhea can be symptoms of diabetes. If any violations occur in the work of the gastrointestinal tract, if there is a CD, you need to consult a doctor and pass the examination. This may be a manifestation of abdominal neuropathy. The symptoms arising from various pathologies of the gastrointestinal tract on the background of the SD are reduced to the following list:
- constipation / diarrhea;
- heartburn;
- belching;
- severity in the area of \u200b\u200bthe stomach;
- nausea;
- vomiting;
- flatulence;
- stomach ache.
Diagnostics
Diabetics need to regularly check blood sugar levels and regulate this indicator playing an important role in the diagnosis of CD complications. If the patient has a digestion disorder, first of all, the diagnosis of the patient self-control diagnostics is studied. Constantly increased sugar, especially with a long-term course of the disease, indicates the possible development of neuropathy, which provokes gastrointestinal diseases. To form an accurate diagnosis, the following diagnostic methods are applied:
- Collect anamnesis. The patient asked about the complaints, their dependence on the supply, etc.
- General inspection. The doctor checks the presence of a plaque in the language, performs percussion, palpation, auscultation (climbs, provers and listens to the stomach).
- Endoscopy. The hardware method reveals the state of the digestive organs, the presence of inflammatory processes and tumors.
- Manometry. Method of measuring pressure in different parts of the gastrointestinal tract.
- Gastography. The method determines the features and availability of violations of motorcycle gasts.
- Study secretion. With the help of special probes, an intricultural measurement of gastric juice acidity is carried out or the presence of a stomach content for subsequent analysis during endoscopy.
- Ultrasound. Allows you to draw up the overall picture of the state of the body, the method is especially relevant in the diagnosis of liver disease.
Common pathology of the gastrointestinal tract with SD and their treatment
 The frequent phenomenon of diabetics is problems with the gastrointestinal tract.
The frequent phenomenon of diabetics is problems with the gastrointestinal tract. An important role in coordinating the work of the digestive system is played by a wandering nerve. Any damage to the nervous tissue as a result of diabetic neuropathy leads to a violation of the work of the nervous system, which entails a number of complications. The patient develops dysbacteriosis, the stomach and / or intestines begins to hurt, the digestion disorder arises, which worsens overall well-being. In diabetes mellitus, it is possible to develop various gastrointestinal diseases, but several diseases are more often diagnosed.
Diseases of the stomach
Gastroparesis
Pathology is often evolving precisely in people suffering from diabetes as a result of the defeat of the vagus nerve. A distinctive feature of the disease is a violation of the stomach motility and slow motion moving into the intestine. Stagnation is formed in the stomach. As part of the treatment of pathology, the patient is recommended to eat fractionally, and when aggravating the disease, go to liquid food. The following drugs are prescribed:
Prank ulcer
The damage to the mucous membrane of the stomach and esophagus with hydrochloric acid disrupts the digestion. If the bacteria of the chielicobacter pylori in the patient develops a ulcer. Because of the wrong power, gastric juice literally corps the resulting ulcer. In diabetics, pathology is treated in the same way as in people who do not suffer from diabetes. As part of the treatment, items suppressing the secretion of stomach and antibiotics aimed at combating the causative agent of the disease.
If the stomach ache in diabetics and these sensations occur periodically or carry a long time, then this is a unambiguous signal about the development of pathology. Tighten and try to cope with the situation only in such cases dangerous. People with diabetes and so understated pain threshold and if pain is already intensively feeling, that is, the risk of occurrence of serious concomitant diseases.
For what reasons may abdominal pain arise?
The increased content of glucose in the blood is reflected in many metabolic processes, including reactions occurring in the tract and other internal organs. Such phenomena indirectly affect the functions of various systems in the body, which subsequently leads to the unpleasant sensations of various etiology. According to statistics, more than 70% of people with blood sugar levels periodically mark abdominal pain in diabetes and in each case they may be provoked by different factors.
Considering the main reasons that can cause pain in the abdomen, you can allocate:
- Incorrect meals Deviation from diet, fatty dishes or any other products, harmful during glycemia, are able to cause stomach disorders. In some cases, they are short-term and pass on their own, but it is not necessary to ignore them at all and, when you visit a doctor, you must report them.
- The ulcer of the stomach or duodenum. Georce entities often occur due to the walls of the organ of bacterial agents and if the body is not able to prevent the spread of these microorganisms, they begin to multiply, problem foci are formed. Similarly, the most common causes of ulcers - Helicobacter Pilori. In diabetes mellitus, the body lacks its own resources to fight bacteria and medium itself, with an increased glucose content, often becomes favorable.
- Gastroparesis Diabetic or slow digestion of food, its detention in the stomach. This leads to its overflow and subsequent pain, and to other complications.
- Neuropathy. Pathology is associated with damage to nerve fibers, which is reflected on the transmission of signals to the brain, the quality of the flow of metabolic processes. Violations can touch all the intestinal departments, from this problem with the chair, and other phenomena that can cause abdominal pain in diabetes.
- Inflammation or dysfunction of the pancreas. This body is responsible for the development of insulin. If the jackets of the content of this hormone are coming, which often happens. Such phenomena are reflected in digestion and in general on general well-being.
- Violation of microflora, in particular,. The fungal disease can spread to any mucous membrane, and excess sugar contributes to this process. Because of this, pain in the abdomen, a variety of gastrointestinal disorders appears.
- Liver pathology. These may include hemochromatosis, fatty dystrophy, which develops with a particularly overweight patient and in the absence of control leads to an increase in the body.
Provice abdominal pain in a person with hyperglycemia can the same reasons as at the normal level of sugar. The difference is the greatest susceptibility of the organism of diabetics to various external influences, as well as the incorrect flow of a number of reactions in the body.
How to treat abdominal pain?
 When discomfort in the abdomen, it is not necessary to immediately try to stop painting with various painkillers or resort to popular recipes. Provice such a state may have a number of reasons and it is important to determine them, otherwise there is a possibility of aggravation of the situation. If the attack is strong, there is vomiting, an increase in temperature, hiding masses with blood or other critical symptoms take place, then immediately need to cause ambulance. With moderate pain and absence of pronounced symptoms, it is recommended to refer to the therapist or observing doctor.
When discomfort in the abdomen, it is not necessary to immediately try to stop painting with various painkillers or resort to popular recipes. Provice such a state may have a number of reasons and it is important to determine them, otherwise there is a possibility of aggravation of the situation. If the attack is strong, there is vomiting, an increase in temperature, hiding masses with blood or other critical symptoms take place, then immediately need to cause ambulance. With moderate pain and absence of pronounced symptoms, it is recommended to refer to the therapist or observing doctor.
In each case, a certain treatment scheme is selected. It is preceded by a comprehensive diagnostics to find out why stomach ache under diabetes mellitus and is it connected with blood glucose disorders. It may be necessary to change the method of maintaining the blood glucose level, which happens with type 2 diabetes or the insulin dosing will be revised. At the same time, measures are taken to eliminate root causes of abdominal pain, for example:
- A strict diet is prescribed with except fatty food, defiantly meteorism and weight gain.
- Reception of enzymes for the restoration of the pancreas.
- The inclusion of drugs that help restore the normal intestinal microflora.
- The choice of corticosteroids, sedatives, physiotherapy methods, which is shown in the signs of neuropathy.
- Laxative means.
What therapy will be, will depend on the type of disease, but any treatment, especially with diabetes, should be appointed exclusively by the doctor.
Complications of the disease often cause abdominal pain during diabetes mellitus. They can be short-lived as a reaction to food, and indicate pathology. In diabetes, the patient decreases the pain threshold, respectively, pain is already perceived with strong disorders. In such a situation, you need to immediately contact the doctor, which will send to the necessary diagnostics of the SD and the abdominal cavity. The following is prescribed treatment based on the patient's clinical picture. The basis of prevention is the observance of the necessary and moderate physical exertion.
Complications of diabetes that cause pain
With violation of the pancreas and sacchal diabetes occurs in insulin production. Very serious illness, the complications of which lead to irreversible consequences. The painful sensations in the stomach in diabetes are short-term (they are tormented shortly and pass independently) and long-term (sign about problems). Factors provoking pain in the abdomen during diabetes mellitus, are:
- stomach ulcer and 12 pans;
- reaction to drugs with metformines (due to a lack of calories in food) and use when drinking alcoholic beverages;
- acidosis lactic acid;
- liver ailments;
- ketoacidosis;
- chronic hepatitis.
It should be understood that the feeling of pain in diabetics is dulled, and if it is manifested by such a symptom, it means that difficult complications occur in the body that require immediate clinical assistance.
Diagnosis of abdominal pain in diabetes
To establish the cause of unpleasant sensations, prescribe an abdominal ultrasound.
Install the cause of abdominal pain at the SD is independently impossible. For this, a number of laboratory studies are carried out. The priority is to find out the feeling of the patient, which preceded the appearance of symptoms when diabetes began. To do this, conduct an oral survey, palpation and inspection of the patient. Next, the sugar level is measured, the glycemic profile is found out, insulin indicator. A test for glucose tolerance is carried out and the level of glycosylated hemoglobin is measured. Blood biochemistry (laboratory analysis) and urinary analysis, rebarga test and ultrasound examination of abdominal organs.
ECG, measuring the level of acetone, the electrolyte composition of the blood is done if necessary. Only after these manipulations, the attending doctor will be able to see a complete clinical picture and prescribe treatment. Diagnostics may not be limited to described analysis, but to include additional research related to painful sensations. The direction to the diagnostic procedures gives the attending physician, based on the history of the disease and the responses of the patient.
Treatment and prevention
Treatment of diabetes mellitus includes balance of sugar levels and normalization of metabolism. Manifestations of concomitant pain in the abdomen can be reduced. For this, doctors prescribe permissible painkillers. It is important to get rid of the illness causing pain and continue insulin treatment of diabetes. An important step in treatment and prevention is meal:
- adjusts the mode of meals;
- products are excluded with a high carbohydrate content;
- it is prohibited fatty, acute, harmful food, confectionery and sweet drinks.
For the prevention of complications of the main disease, it is important to control blood pressure indicators.
To prevent the complication of diabetes and associated diseases that cause abdominal pain, it is necessary to systematically undergo an inspection from the endocrinologist and make independent measurements of the level of sugar. Rest, moderate physical exertion contribute to the speedy recovery. It is important to observe the indicators of blood pressure and not to leave the accompanying diseases are unreacted. Under any deviations, it is impossible to postpone the visit to the doctor. Synthetic drugs are prescribed by an exclusively attending doctor.
The actual problem of clinical medicine was and remains the problem of false acute abdomen (s). Pateogenetic mechanisms of lies are quite complex, diverse and individual in each case. Traditionally, it is believed that one of the causes of the lies is complicated flow of diabetes (SD) with a significant impact of exchange in the presence of hyperglycemia and ketoacidosis, as a result of which the inflammation of the peritoness (aseptic peritonitis) is developing with the peritonism clinic.
We have 6 cases when the days developed with a long history (5-10 years) SD II type II with the development of complications (and concomitant pathology) in the form of: diabetic nephropathy, cardiomyopathy, gastro-party, vegetative neuropathy and their subsequent combined flow, but without hyperglycemia and ketoacidase. The age of patients was from 53 to 78 years, there were 5 women and 1 man.
The purpose of the article - clarify the pathogenetic mechanisms for the development of lies in the cases we observe
Example 1. Patient B., 53 years old, entered 1 HIR. Department with diabetes: acute belly (?), type II diabetes, serious degree, dia-trifer nephropathy, cardiomyopathy, hypertensive disease, double-sided hydrotox, chronic colitis.
With complaints about pain in the epigastrium, which moves into both hypochondrians, the pain is high in the epigastric corner and in the left lower half of the abdomen, nausea, vomiting, dry mouth, lack of appetite, weakness, random-gas. Also, the patient was disturbed by pain in both lower extremities, parastzia. The patient is significantly astheniced, dried, and hypochondria.
In history: it suffers from diabetes 10 years, sugar corrigar is a reception of diabeton tablets, suffers from constipation of 4-5 days, the chair is usually after receiving laxatives; Appendectomy 8 years ago. A month ago, lay in the therapeutic hospital and received conventional treatment for CD, diabetic nephropathy, hypertonicity, cardiomyopathy. Was discharged with improvement. After 3 weeks after discharge, the state worsened again and the patient again appealed to the clinic.
Objectively: skin covers expressed pale. Pulse 92 wt. per minute, hell 130/80 mm.rt.st. There is a small shortness of breath. Language is moderately dry, covered with a white bloom. The belly will be moderately evenly, participates in the act of breathing. With surface palpation, soft. With deep palpation, it is moderately straining in all the departments of the abdomen, especially in the right hypochondrium, where the speaker on 2-3 cm is flat, the painful edge of the liver is palpable. Palpation is also painful in epigastrics, in the aircraft region and in the left lower half of the abdomen. Percussively, above the left lower half belly - tympanitis. Intestinal peristalsis is weakened. The moderate swelling of the legs is determined.
The percussion of the back gives a dullness of the percussion sound over the lower chest departments and loose breathing there. With a state-made FGS - a picture of surface gastritis, bulbite.
Ultrasound: In both pleural cavities, a significant amount of fluid. In the abdominal cavity, a small amount of liquid. The liver is diffuse, increased by 2.5 cm and due to fluid in the pleural cavity protrudes from under the rib arc by 5 cm. Gallbladder: Walls are eaten, there are no stones. The spleen is not enlarged. Kidneys: Parenchima Hydrophilicity, urine outflow is not broken.
With an x-ray-study of the chest: double-sided hydrotrox, fluid level on the right - VII edge, left VII - VIII edge, rear account.
Analysis data. General blood test: hemoglobin-80g / l, ER-2.9 million, CP-0.9, leukocytosis-6.2 thousand, RO-8 mm / hour.
General urine analysis: Specific weight 1.018, transparent, protein 0.38%, leukocytes 2-4 in P / view, Erythrocytes - 0-1 in P / view. Blood sugar Colace from 4.5 to 9.4 mmol / l. Biochemical blood test: total protein -61.9 g / l, (N 65-75); Bilirubin 16.2 (free-13.1, associated-3,1), Alt 22.0 (n to 40), AST 16 (n to 40). MODE-11.0 (N 2.5-8.3 ), Creatine-225 (No. 91-115).
Electrolytes: Potassium-3.24 (N 3.5-5.0), sodium-132.5 (N 136-146), calcium 1.04 (N 1.05 - 1.27). Urine tests for sugar and acetone negative.
According to laboratory analyzes, we have anemia, small hypoproteinemia (like manifestations of intoxication), blood sugar is slightly higher than the upper limit of the norm, sugar and urine acetone negative.
Thus, the severity of the state was determined not by exchange disorders (no hyperglycemia and ketoacidosis), and intoxication phenomena.
A pleural puncture was made and the right of 700 ml was evacuated, on the left -500 ml of serous effusion. Cleaning enema was made, after which there was a small intestinal action, gases were moved, the abdomen decreased.
Treatment: Correction of sugar injections insulin, intravenous transfusion of physical. solution, in / in quamatel, essential, in / m - spasmolgon; Phospholyugel, after which the patient noted the relief of the condition: abdominal pain decreased, vomiting ceased, nausea decreased. The next day, pain in the stomach and nausea was completely passed.
Based on the complaints of the patient: nausea, vomiting, the feeling of bloating, constipation, objectively determined by a moderate uniform swelling of the abdomen, as well as auscultative - the weakening of the peristaltics of the kishchek-nickname, one can assume that the leading pathogenetic mechanism, the C-Muling Clinic of Acute Abdomen, was Violation (oppression) of the motor-evacuation function of the gastrointestinal tract.
Stretching the colon, as well as an increase in liver with a growing capsule, was the cause of abdominal pain. The presence of hydro-toroxes on both sides aggravated by a severe condition of the patient and the occurrence of shortness of breath.
Example 2. Patient N., 60 years old, entered nephrological leases with complaints of nausea, dry mouth, general weakness, random-gas. These complaints appeared 4 days ago and improved progressively. In the history: 10 years suffers from type II diabetes, (sugar corrigs - with 1 tablet of diabetes), diabetic nephropathy, hypertonicity. In 1990, he suffered appendectomy, in 1991- ammputation of the uterus. In 1997, it was operated on about acute intestinal obstruction, in 2007 - laboratory cholecystectomy.
In the history, in December 2009 lay in the gastroenterological department with complaints of pain in the epigastric region, nausea, vomiting. Then there was an increase in hell. Diagnosed: aggravation of DPK ulcers, chronic erosive gastritis, type II SD, hypertensive disease.
Conservative treatment was started in the department, but the condition has progressively deteriorated, IKOT, jeeping, repeated vomiting, abdominal pain. There was a suspicion of an acute surgical disease, the patient consulted the surgeon. The patient's condition is severe, restless. Patient of good nutrition, skin pale with eartling tint. The belly will be moderately evenly, participates in the act of breathing. On the anterior abdominal wall, the scars after appendectomy, gynecological surgery (transverse scar of the PFFANENSTIL) and a transrectal - for adhesive intestinal obstruction. With palpation, the belly is soft, painful high in the epigastric corner, the liver is increased, protrudes from under the rib arc by 2-3 cm, the edge is rounded, moderately painful. There is a moderate swelling of the legs. In the patient 4 days there was no chairs. It also turned out that before it was disturbed by belching, jeeping, periodically - heartburn during slopes and night (slept on the low pillow).
Hell-130/70 mm.rt.st. Blood sugar is 7.6 mg / l; Urea-5.7, Creating Ning-97,1. Bilirubin 16.6, free-14.5, bound-2,1, AST-54 (n to 40), Alt-62.0 (n to 40).
During admission, an ultrasound was made: the liver is increased by 1.5-2 cm, diffusely changed by the type of body hepatosis. Gall bubble removed. Pancreas is diffusely changed. Spleen without features. The kidney on the right is 9.2 by 3.4 cm., Left 9.7 to 4.5. Parenchima is diffusively changed, thinned, the surface is uneven. The thickness of the guy chims is 0.8 per 1.0 cm. There are no stones. Kidney shrouded. Bladder without features.
The presence of an acute abdomen with the phenomena of acute intestinal obstruction was suspected, however, with an x-ray study, the casing-ber and / or air arches were not detected. Given that the stomach is soft, painful only high in the epigastric corner, as well as data X-ray studies, acute belly was excluded.
With FGS (the next day), the presence of hernia of the food-aqueous hole of the diaphragm (GPO), atrophic gastritis, duodenitis is established.
Diagnosed: SD, diabetic nephropathy, hypertonicity, sickness, guy, adhesive disease, parires of the upper sections of the gastrointestinal tract.
The patient was translated into the intensive care unit, the intestinal stimulation was carried out, infusion therapy, the correction of sugar. Prescribed quamatel (in / c), Cerukal (in / m), phospholyugel, Gaviscon. The patient's condition gradually normalized, vomiting ceased.
It is believed that changes in the engine-evacuation function of the stomach and DPK largely determine the pathogenetic mechanisms and the clinical features of the development of the diseases of the tract (4). In this example, Icota, tightening, repeated vomiting, abdominal pain, in the presence of postoperative scars on the anterior abdominal wall and a moderate abdomen, indicated that the leading pathogenetic mechanism simulating the clinic of the lodges (as in the previous case) is a violation (oppression) Motor-evacuator function of the gastrointestinal tract. An additional role was played by the presence of HPD (for which the presence of gastric hypomotoric with functional duodenostasis (2), as well as chronic gastritis and duodenitis.
In the two cases that we have given the most characteristic of the patients who understand the patients, the presence of an acute surgery of the abdomen (the cause of which is inflammation and / or the destruction of the gastrointestinal bodies), but subsequent observation and treatment has made it possible to exclude acute abdomen and diagnose Lies, that is, the changes were functional (reversible). As is known, the cause of abdomy-low pain in functional disorders of the GTS is the torment of the motor function of the tract and changing the sensitivity of the receptor-node machine. Considering that in prolonged, complicated flow of the CD, vegetative neuropathy and encephalopathy observes, it can be assumed that one of the reasons for the occurrence of abdominal pain in the cases was a decrease in the threshold of the sensitivity of the receptor nervous apparatus of the gastrointestinal tract, along with the violation of the motor function of the gastrointestinal tract.
Thus, the leading cause of lies at the SD in the cases we understand:
- oppression of motorcycle gasts;
- reducing the threshold of the sensitivity of the receptor apparatus, with a significant asthenization of patients and often their ashivat, due to chronic intoxication (without ketoacidosis). At the same time, in the cases, the presenter pathogenetic mechanism of the lies is significantly different from the lies at the SD with ketoacidosis.
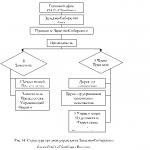
Briefly pathogenesis of LD at SD in the above cases can be represented as follows.
Long flow of type II (5-10 years). Complications of SD: microangiopathy, diabetic hepato-nephropathy, cardiomyopathy, vegetative neuropathy, encephalopathy, (with gastro-entero-chopathy, gastritis and duodenitis phenomena) and their subsequent shared flow with integrated syndrome. With:
- insufficient treatment or at the initially detected SD;
- concomitant pathology (gpod, gynecological, etc.);
- transferred operations in history (adhesive disease).
Asthenization of the body. Due to chronic intoxication, which was manifested in the form of anemia, hypoproteinemia; urea, creatinine just above the upper limit of the norm; Alt, AST in N or slightly above the upper limit of the norm, with sufficient compensatory mechanisms.
Reduced immunity. Cold, viral diseases, which is a row aggravation of the disease.
Decompensation of the protective forces of the body. Significant oppression of the motor-evacuatorial function of the gastrointestinal tract at all of its levels: F-K, DPK, thin and fat intestines
Reducing the sensitivity of pain receptors.
False acute belly. Pain in the stomach, bloating, Tosh note, repeated vomiting, the general serious condition of patients
Based on the foregoing, the following conclusions can be drawn.
Findings:
- False acute stomach may be a consequence of not only complicated flow of SD with hyperglycemia and ketoacidosis, but also a complicated flow of SD without glycemia and ketoacidase (without significant exchange disorders), but with a long history with complications (diabetic hepatoma neuropathy, cardiomyopathy, vegetative neuropathy) in combination with concomitant pathology (or complications) in the form of gastroduodenitis, chronic colitis, hydrophole, as well as adhesive disease and hydrotox.
- The leading pathogenetic mechanism in the disassembled cases can be considered the oppression of the motor-evacuator function of the tract and the reduction of the threshold of pain sensitivity, with significant asthenization of the organism due to chronic intoxication.
- Based on such an understanding of the pathogenesis of Lodi, the treatment of the paragraph should include disinfecting therapy, along with the saccharine of sugar, as well as prokinetics (with local intestinal stimulation), antisecretory and anatacid therapy. All of the above allows you to remove intoxication, normalize the motor-evacuator function of the gastrointestinal tract, fairly quickly facilitate the condition of the patients and eliminate the sharp belly.
- The presence of adhesive disease can be considered a factor in predispo-lagging to the occurrence of lies. The complicated course of hydrocytoxes and collides, as well as the presence of hydrotrox (large and medium-sized), are provoking (resolved) factor in the occurrence of lies, so they need their adequate treatment.
Literature
- Belusova E., Zlatkin A.R. Abdominal pain with functional gastrointestinal disorders: basic mechanisms and removal paths. // South Russian Medical Journal. - 2002.-№ 2.-C-51-58.
- Vakhrushev Ya.M., Potapova L.O. Functional state of the gastroduodenal zone with gastroesophageal reflux disease. // Executive. and wedge. Gastronth. - 2007. - No. 3. - from 22-26.
- Evyukhov R.M., Gryaznova S.N., Vorobev V.P. To the diagnosis of pseudo-peritoneal syndrome. // Wedge. MED. - 1986.-№ 10. - C 110-114.
- Maev I.V., Samsonov A.A., Vorobev L.P. et al. Secretory, motor functions of the stomach and duodenal intestine, duodenogastral reflux in patients with ulcerative duodenal disease. // Wedge. Honey. -2000.-№ 6. - C 39-42.
- Mazowiecksky A.G., Velikov V.K. Cartoon diabetes. M. Medicine. - 1987.-C 288.
- Frolkis A.V. Functional diseases of the gastrointestinal tract. - L. Medicine.-1991.-C 221.
- Zimmerman Ya.S. Abdominal pain syndrome: issues of etiology, pathogenesis, diagnosis and treatment. Wedge. MED. - 2010.- №2.- from 14-21.