Invasive and non-invasive methods for registering blood pressure. Invasive blood pressure monitoring
Invasive measurement arterial pressure - The most accurate method of monitoring blood pressure indicators, which is carried out directly in line with blood flow. The procedure is carried out by introducing the needle to the artery and connecting through the system of the tubes to the manometer. Such a method is practiced during surgical intervention or when performing resuscitation manipulations, as it helps to track any changes in real time pressure.
It is possible to measure arterial pressure with an invasive method using a special catheter installed in the arteries, only in the hospital under the hospital under the non-primary control of medical workers.
The method of invasive measurement of blood pressure is characterized by absolute accuracy, but can not be practiced constantly. The procedure is sufficiently painful and trauma, after it there is a risk of developing complications, so the method applies only in exceptional cases.
Direct measurement of blood pressure is practiced when time is not enough to carry out a standard, non-invasive, manipulation with the dinging of the cuff and air pumping. This allows you to quickly get the most complete picture of the status. of cardio-vascular system while doing surgical operationsWhen any delay can cost a patient of life.
Indications for invasive measurement:
- carrying out a surgical operation;
- controlled hypotension;
- intense artificial ventilation of the lungs;
- cardiogenic shock;
- stay in intensive care.
The method is shown to patients with unstable hemodynamics, as it allows you to constantly track any changes in blood flow. In this case, the artery catheterization and connection to a special instrument for measuring pressure allows you to promptly detect any deviations in the work of the heart and take therapeutic measures on time.
The direct method of measuring pressure is practiced in the separation of intensive therapy of maternity houses. Usually, such a procedure is exposed to strongly premature children. The system is installed in the umbilical artery.
The use of the method during surgical intervention makes it possible to reduce the risk of developing sudden heart complications. Constant pressure monitoring in this case helps to take measures in a timely manner at risk of brain stroke, myocardial infarction, critical pressure change.
Preparation for the procedure
Allen's sample need to determine the possibility of the procedure
Preparation comes down to conducting the sample of Allen and sterilization of tools. The catheter or cannula is installed in one of the following arteries:
- ray;
- elbow;
- shoulder;
- femoral;
- mortar.
Allen's sample is a quick method for determining collateral blood circulation. This test is necessary, since some people have a violation of collateral blood flow, which does not allow you to enter the catheter in the radiation artery.
In 90% of cases, the beam artery catheterization is carried out due to its surface location.
The elbow artery can also be used to conduct manipulation, but there is a risk of damage to it, which entails a breakdown of the brush. The elbow artery occurs deeper than radiation, so the installation procedure of the catheter is significantly complicated.
The catheter can be installed in the shoulder artery. In this case, the measurement results are quite accurate, as it passes near the aorta. The minus is that when installing the sensor, distortion is possible due to the movement of the hand, which lead to the rigging of the catheter.
The femoral artery for monitoring the Hell is a direct method of measuring blood pressure used in extreme cases. This is due to the greatest risk of developing complications.
The measurement of blood pressure in the axillary artery is practically not practically practiced due to the risk of damage to the nerve endings and the development of brain vessels by the irregular washing of the catheter.
An important phase of preparation for the procedure is an assessment of the possibility of installing a catheter in the artery. Main preparatory stages:
- artery availability assessment;
- check collateral blood flow (allen sample);
- determination of the diameter of the catheter and the ratio of it with the size of the artery.
The place to install the catheter is selected in such a way as to avoid the risks of the secrets and fluids of the body to the area of \u200b\u200bthe puncture of the arteries.
Invasive pressure measurement is carried out only in critical situations. Despite high risks The development of complications, often the only available place remains femurful artery, for example, with extensive burns or after accidents.

The catheter can be installed in one of several arteries.
How is the invasive measurement of hell?
The procedure is carried out under local anesthesia if the patient is conscious. This is necessary in order to minimize pain when skin crossing and installing the catheter. Typically, this is used by lidocaine. The artery establishes a catheter, which with special System The tubes are connected to the sensor. A special solution is flowing on the tubes that preventing the collapse of the blood and ensures the transmission of oscillations on the invasive pressure sensor.
The sensor capturing blood pressure fluctuations should be installed at the heart level in the so-called "zero" point. The sensor takes fluctuations in blood, converts them to an electrical signal, understandable to a computer, which is then displayed on the monitor. On the screen, you can track the dynamics of changes in blood pressure in the form of a curve.
Rules for the procedure:
- the definition of a "zero" point, which corresponds to the level of the heart;
- at the height of the "zero" point, an adapter is installed above the sensor;
- the adapter is connected to the patient's limb;
- the monitor is calibrated "Point of Heart".
After these events, the doctor presses the inclusion button and the process of continuous pressure measurement begins. If necessary, the temporary framework of sound alert is set. When fluctuations in pressure and critical changes, the hell is a loud beep.
When conducting the procedure, it is important that the patient constantly remains under the supervision of medical personnel. The liquid that flows across the tubes changes every day. Usually, with invasive blood pressure measurement, the usual sodium sodium physical physios is used, however, in the overdose of sodium, the blood pressure may rise in a certain category of patients, so the solution can be replaced with glucose. The catheter must be changed every 24 hours, while the staff should keep track of the air to the artery. When forming blood clots, their removal is carried out, in order to avoid the development of dangerous complications.
Since the measurements are carried out on the limbs, it is important to monitor the condition of the skin of the fingers. If the catheter is incorrect installation, blood flow is disturbed, which can lead to the sinusiness of the fingers and the impaired sensitivity.

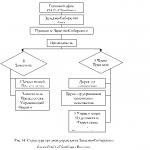
Schematic image of the procedure
Contraindications
When the pressure is measured by an indirect method for determining the blood pressure using contraindication tone meters, there is practically no, unlike the direct method of measuring blood pressure.
Invasive blood pressure measurement is not carried out with pronounced vascular failure and Reyno syndrome. In any case, the decision on the need for invasive monitoring of Head adopts a doctor on the basis of a patient survey and after assessing the overall condition of the body. The procedure itself is quite traumatic and dangerous, so monitoring is associated with severe risks not only for health, but also for the life of the patient.
Possible complications
Complications and risks of the procedure depend on the installation site of the catheter. In general, manipulation is dangerous by the development of thrombosis and air bubbles in the vein when installing the catheter or cannula. When installing the cannula in the femoral artery there is a risk of development:
- aseptic necrosis;
- thromboembolism;
- severe circulatory disorders in the legs;
- loss of fingertips;
- pseudoianevrisms;
- atteroma.
Installing the catheter in the radiation artery can lead to the same complications. When measuring pressure through the elbow artery, there is a risk of developing heavy blood flow disorders in the brush with further loss of fingers. If the manipulation is carried out by puncture of the axillary artery, there is a high risk of impairment sensitivity due to damage to nerve endings.
Violation of the course of the procedure may cause spasm artery, hematoma, thrombosis, ischemic necrosis.
It is possible to minimize the risk of developing hazardous complications with careful preparation for manipulation - it depends primarily on the professionalism of the doctor.
The cannulating of the arteries allows for continuous monitoring of the heart rate and blood pressure, which is necessary in patients in the intensive-anesthetic separation of inetropic therapy or with hemodynamic instability. Intraoperative monitoring should also be carried out with a patient with a high risk of complications from the cardiovascular system. We would place arterial types in the preference of their use as follows: radius\u003e Poor\u003e Stop Real\u003e Middle. We recommend cannorate the ray artery and artery of the rear of the foot "fast" catheters or intravenous angiocateurs, and for the femoral and axillary arteries, use the Mercider's methodology.
Beam artery cannulation
Indications:
Permanent monitoring of hemodynamics.
Contraindications:
Negative Test Allen:
Turn the elbow and radiation artery with your fingers so that the blood on the veins spacked out of the brush and the latter pale.
Free the elbow artery by continuing to press the radiation artery.
If the hand color does not return to the initial 5 second, the test allen is considered negative, which indicates an occlusion of radial artery.
Anesthesia:
1% lidocaine.
Equipment:
Angicategher 20 caliber or "fast" catheters.
Suture material.
Heparinized system for washing with monitoring sensors.
Sterile bandages.
Hand towel.
Antiseptic solution.
Needle 25 caliber.
Position:
The brush in the palm position upwards dismissed in the rays-up joint, is placed on the wrist on the rolled towel rolled. Fix the palm and forearm to stand for hand.
Equipment:
Proceed by antiseptic and steroid sterile napkins the skin of the inner surface of the wrist.
Palpise the pulse on the radial artery at the distal end of the radial bone.
Anesthetize the skin with a needle of 25 caliber above this point.

Point the skin of the angiocateter 20 caliber is upward, directing the needle at an angle of 45 ° to the skin surface. Adjust the angiocateter in the direction of the palpable pulse before the blood appears from the needle.

If blood does not appear,slowly remove the angiocateter and again enter it at an angle of 60 ° toward the pulsating artery.
If there is a good reverse blood flow,adjust the angiocateter forward by 2 mm to provide its intraarterial location. If you use a "fast" catheter,these additional 2 mm are not necessary, in this case, promote the conductor of the catheter in the artery.
Remove the needle I. press your fingerthe proximal radiation artery department for preventing excessive bleeding.
No bleedingit indicates that the catheter is not in the arms of the artery. Slowly remove the catheter. In the event that the rear wall of the artery is punctured, blood from the needle will appear. If blood is not, remove the catheter by pressing the point of puncture to 5 minutes.
Complications and their elimination:
Low amplitude of blood pressure waves: Check all connections and cranes on the tube system. Exclude the external proximal compression of the artery. Check the position of the hand and wrist. The hand should not be raised, and the wrist should be dispersed. If the amplitude of the blood pressure waves is low and the blood flow from the catheter is weak, move the catheter.
Ischemia fingers brush: Remove the catheter and carefully observed for the state of the fingers.
Caution Tar Caution Foot
Indications:
A frequent estimate of the gas composition of arterial blood.
Contraindications:
The pulse on the artery of the rear of the foot is not determined.
Anesthesia:
1% lidocaine.
Equipment:
Antiseptic solution.
Sterile gloves and napkins.
Needle 25 caliber.
Syringe 5 ml.
Angicateter 20 caliber (2 ") or" fast "catheters.
Suture material (Silk 2-0).
System for intravenous infusion with a device for creating pressure in the system.
Sterile bandages.
Position:
Foot in neutral position.
Equipment:
Process with antiseptic solution and sterile the sterile material of the back surface of the foot.
Plut the pulse on the artery of the rear of the foot laterally long extensor thumb Foot at the level of the first metallic-wedge-shaped joint.
Anesthetize the skin above this point using a 25 caliber needle.
Pulit the skin of the 20 caliber angiocateter 20, directing the needle at an angle of 45 ° to the skin surface. Promote an angiocateter in the direction of the pulsating vessel until blood appears from the needle.

If blood does not appear, slowly remove the angiocateter and again enter it at an angle of 60 ° to the palpable pulsating vessel.
If there is a good reverse blood flow, push the angiocateter forward to 2 mm to provide its intraarterial location. If you use a "fast" catheter, these extra 2 mm are not necessary, in this case, promote the conductor of the catheter in the artery.
I reliably holding the needle of the catheter, slowly push the catheter to the artery.
Remove the needle and press your finger the proximal radiation artery department to prevent excessive bleeding.
The absence of bleeding indicates that the catheter is not in the lumen of the artery. Slowly remove the catheter. In the event that the rear wall of the artery is punctured, blood from the needle will appear. If there is no blood, remove the catheter, pressing the place of puncture for 15 minutes . Specify the guidelines and try again to perform steps from (4) to (8).
If the puncture succeeds, install the system for infusion and attach the sensors to the monitor; Evaluate the form of blood pressure wave.
Fix the catheter to the skin of the silk seams and impose a sterile bandage.
If three catheterization attempts turned out to be unsuccessful, stop the procedure and try cannorate the artery on the other side.
Complications and their elimination:
Low amplitude of blood pressure waves: Check all connections and cranes on the tube system. Exclude the external proximal compression of the artery. If the amplitude of the blood pressure waves is low and the blood flow from the catheter is weak, move the catheter.
Stop's fingers ischemia: Remove the catheter and watch your fingertips carefully.
Caution of the femoral artery
Indications:
Long monitoring hemodynamics.
A frequent estimate of the gas composition of arterial blood.
Introduction of an intra-director balloon pump.
Contraindications:
The presence of an iliac or femoral arterial vascular transplant (prosthesis).
Operations in the area of \u200b\u200bgroin in history (relative contraindication).
The patient must be in bed until the catheter is extracted.
Anesthesia:
1% lidocaine.
Equipment:
Antiseptic solution.
Sterile gloves and napkins.
Needle 25 caliber.
Syringe 5 ml (2).
Catheter (6 ") 16 caliber.
0.035 J-shaped conductor.
Sterile bandages.
Safe razor.
Suture material (Silk 2-0).
System for intravenous infusion, a device for creating pressure in the system.
Heparinized system for washing with monitoring sensors.
Position:
Lying on the back.
Equipment:
Early, treat with antiseptic solution and sterile the left or right ink area with a sterile material.
Plut the pulse on the femoral arteries in the middle point on the imaginary segment connecting the Luma Symphysia and the front upper robe. Follow the pulsating artery by 1-2 cm distal than (point A).
Enter anesthetic through the needle 25 caliber in the skin and subcutaneous tissue along the type of artery.
18 caliber puncture needle with a syringe of 5 ml. Pulit the skin at a point A and advance the needle in the cranial direction, at an angle of 45 ° to the surface of the skin, towards the pulsating vessel, supporting the peccation in the syringe.

If the blood current is not obtained after passing to a depth of 5 cm, slowly remove the needle by supporting the peculiarity in the syringe. If the blood in the syringe did not appear, again send the needle to the palpable pulse, slightly changing the direction of its movement.

If arterial blood appeared in the syringe, recheck the benchmarks and try to conduct puncture at a point located per 1 cm proximal than the point and in the course of the artery as described in (4 p.). If the attempt turns out to be unsuccessful, stop the execution of the manipulation.
If the needle passed into the clearance of the arteries, disconnect the syringe and hold the needle cannula with a finger to prevent excessive bleeding.
Enter the J-shaped conductor through the needle towards the heart, keeping the needle in the same position (Merdinger's method). The conductor must pass with minimal resistance.
Carefully expand the puncture hole with a sterile scalpel.
Remove the conductor and attach the system for washing and sensors to the monitor to estimate the form of the blood pressure curve. Fix the catheter to the skin with silk seams. Take sterile dressing on the skin.
The patient must be in bed until the catheter is removed.
Complications and their elimination:
Punching of femoral veins:
Thrombosis: Remove the catheter. Carefully monitor the pulse on the line of the lower limb to diagnose the distal embolism in a timely manner.
Hematoma: Remove the catheter. Press the place of puncture for 15-20 minutes. Put the tight bandage to this place for another 30 minutes. Bed regime for 4 hours. Control of the pulse on the arteries of the lower limb.
Caution of the axillary artery
Indications:
Long monitoring hemodynamics.
A frequent estimate of the gas composition of arterial blood.
Access for arteriography research.
Contraindications:
The inability to take the hand.
Bad distal peripheral pulse on radial artery.
Anesthesia:
1% lidocaine.
Equipment:
Antiseptic solution.
Sterile gloves and napkins.
Needle 25 caliber.
Syringe 5 ml (2).
Catheter (6 ") 16 caliber.
Penalty needle 18 caliber (5 cm long).
0.035 J-shaped conductor.
Sterile bandages.
Safe razor
Suture material (Silk 2-0).
System for intravenous infusion with a device for creating pressure in the system.
Heparinized system for washing with monitoring sensors.
Position:
Lying on the back, the hand is completely allocated, the shoulder rotates the dust.
Equipment:
Early, treat with antiseptic solution and sterile the axillary area.
Plut the pulse on the axillary artery as proximal and closer to the big thoracic muscle.
Enter anesthetic needle 25 caliber in the skin and subcutaneous tissue along the artery.
The needle for puncture of the artery 18 caliber with a syringe of 5 ml Point anesthetized skin and advance the needle at an angle of 45 ° to the skin surface towards the pulse, supporting the pouring in the syringe.
If the reverse blood flow is not obtained after passing to a depth of 5 cm, slowly remove the needle, supporting the resolution in the syringe. If the blood did not appear, reiterate the needle towards the pulse.
If the blood in the syringe is still no, recheck the guidelines and try to puncture at a point by 1 cm distally in the course of the artery as described in (4 p.). If the attempt is unsuccessful, stop the execution of manipulation.
If venous blood appeared in the syringe, remove the needle, press the place of puncture.
If arterial access is obtained, disconnect the syringe and press the needle hole with your finger to prevent excessive bleeding.
Enter the J-shaped conductor through the needle towards the heart, keeping the position of the needle. The conductor must pass with minimal resistance.
If resistance met, remove the conductor, specify the position of the needle aspiration in the syringe.
As soon as the conductor passed, remove the needle, constantly controlling the position of the conductor.
Expand the puncture hole with a sterile scalpel.
Enter the central venous catheter on the conductor in the artery.
Remove the conductor and attach the system for washing and sensors to the monitor to estimate the form of the blood pressure curve. Fix the catheter to the skin with silk seams.
Take sterile dressing on the skin.
Complications and their elimination:
Vienna puncture: Remove the needle. Press the place of puncture for 10 minutes.
Thrombosis: Remove the catheter. Carefully monitor the pulse along the type of artery and watch the signs of the ischemia of the fingers.
Damage to the shoulder plexus: Remove the catheter. Control sensitivity and motor function. If there is no improvement, call the neurosurgeon for consultation.
Systemic blood pressure
1. What is systemic blood pressure? Systemic blood pressure (garden) reflects the amount of force acting on the walls of large arteries as a result of heart cuts. The garden depends on cardiac output and systemic vascular resistance. When describing the garden usually consider 3 components:
1. Systolic blood pressure - pressure generated by a reduction in heart (or systole);
2. Average blood pressure - average pressure in the vessel during heart cycledetermining the adequacy of perfusion organs;
3. The diastolic blood pressure is the smallest pressure in the arteries during the phase of the phase of the heart (diastole),
2. Why is it so important to measure the garden?
With acute states (injury, sepsis, anesthesia) or chronic diseases (renal failure) often observed the Garden changes. In animals in critical condition, the garden is maintained in the normal limits of compensatory mechanisms until severe disorders occur. Periodic measurement The garden in combination with other routine studies allows you to identify patients with the risk of decompensation at the stage when resuscitation is still possible. In addition, the garden control is shown during anesthesia and when prescribing drugs affecting blood pressure (dopamine, vasodilators).
3. What are the magnitudes of the normal garden?
PRESSURE
Systolic
Diastolic
Average arterial
Dogs
Cats
100-160 mm Hg. Art.
120-150 mm RT. Art.
80-120 mm RT. Art.
70-130 mm RT. Art.
90-120 mm Hg.
100-150 mm RT. Art.
Average blood pressure can be approximately calculated by the formula:
Average hell \u003d (syst. Hell - diast. Hell) / 3 + diast. HELL.
4. What is hypotension?
Average hell< 60 мм рт. ст. отражает состояние гипотензии и свидетельствует о неадекватной перфузии почек, коронарного и церебрального сосудистого русла. Причины развития гипотензии: гиповолемия, сепсис и кардиогенный шок. Клинические признаки гипотензии не специфичны и включают угнетение ЦНС, слабый пульс и тахикардию. Для предупреждения необратимого повреждения органов животного и, как следствие, его смерти требуются быстрое выявление и проведение соответствующих лечебных мероприятий.
5. What is hypertension?
Hypertension is a condition in which an animal in the late garden\u003e 200/110 mm RT. Art. (systolic / diastolic) or average Hell\u003e 130 mm Hg. Art. (Average: 133 mm Hg. Art.). In small animals, the so-called bologne hypertension is found, so pressure indicators must be reproducible and ideally combined with clinical symptoms. Hypertension arises as a result of improving cardiac output or increase systemic vascular resistance and can develop as a primary violation or due to various pathological conditions, including heart disease, hyperthyroidism, renal failure, hyperadrenoxticism, feochromocytoy and painful syndrome. Unckengering hypertension can lead to retinal detachment, encephalopathy, acute vascular disorders and deficiency of the function of various organs.
6. How do the garden measure?
The garden is measured by direct and indirect methods. With direct measurement, the garden in the artery placed the catheter (or needle) and connect it with the pressure converter. This method is the "Gold Standard" when determining the garden. Indirect measurement The garden is carried out using an oscillatry or ultrasonic method of doppler over the peripheral artery (chapter 117).
7. How do direct measurement of the garden?
The garden can be measured constantly if you install a catheter in the dorsal prelice artery, which is usually quite easy to do from any animal with a palpable pulse and weighing more than 5 kg. The arterial catheter is introduced either through the skin, or through a surgical incision. For percutaneous administration of the catheter, the skin area over the dorsal preluduous artery is littered and treated with an antiseptic. The artery takes place in the groove between the 2nd and 3rd prelunduous bones. Before starting the manipulation, the arterial pulse is crushed. Typically use a catheter on a 4 cm length (size 22 or 24 for small dogs), which is administered at an angle of 30-45 ° directly above the palpation site of the pulse until the current of arterial blood is obtained through the catheter. Then the catheter is moving forward, and the stilette is removed. The catheter is fixed according to the standard method of fixing intravenous catheters.
The arterial catheter differs from venous not only by the fact that with its formulation, there is a greater risk of "trusting", but also difficulties in the introduction of fluid into the catheter and maintaining its passability. The arterial catheter needs to be washed with a heparinized solution every 4 hours and from time to time to check its location.
To measure the garden after the arterial catheter formation, the pressure sensor and monitor are used. Many commercial electrocardiographs are adapted to measure pressure. Pressure sensor is connected to the monitor; In this case, the pressure transducer must be approximately at the level of the animal heart. Sterile plastic tubes filled with heparinized solution are connected through adapter taps with a pressure converter and with a patient. The presence of air bubbles is unacceptable in the tubes, otherwise the most minor changes in pressure can be dampy. The use of more rigid tubes provides a smaller change in pressure waves.
Before starting measurements, the system is set to "zero" so that there is no pressure on the converter (i.e., the transient crane is closed), and then the "zero" of the converter is installed in accordance with the instructions for the device. Typically, it is enough to keep the "zero" button down until the "zero" appears on the screen. Then open the tap to the patient and register the pressure curve.
A reliable pressure curve is characterized by a steep rise with a dicrotic recess. If the curve is smoothed, the catheter must be rinsed. If the animal moves during the measurement, you need to re-install the "zero" of the pressure sensor. The first few attempts to form arterial catheters can disappoint the doctor, but soon it will become obvious that their advantages significantly outweigh so obvious inconvenience.
8. What are the advantages and disadvantages of direct measuring garden?
Direct measurement The garden is a "gold standard", with which the indirect methods of registration of the garden are comparing. This technique is inherent not only for measurement accuracy - it makes possible continuous pressure monitoring. Permanent access to the arterial channel allows blood samples to analyze the gas composition in cases where it is required to control the patient's condition.
However, this method has flaws. First, the doctor must perfectly own the professional skills necessary for the introduction and maintenance of the patency of arterial catheters. Secondly, the invasive nature of the formulation of the arterial catheter predisposes to the development of an infection or vessel thrombosis. Third, bleeding is not excluded when the catheter is not excluded during the displacement or damage.
Central venous pressure
9. What is central venous pressure?
Central venous pressure (CVD) is the pressure in the cranial hollow vein or atrium right; which reflects the intravascular volume, heart function and extensibility venous vessels. The orientation of the CTO changes quite accurately characterizes the effectiveness of blood circulation. The CCD is not only a measure of the circulating volume of blood, but also an indicator of the ability of the heart to accept and pump out this volume.
10. How do CVD measure?
The exact measurement of the CVD is feasible only by direct methods. Intravenous catheter introduced into the outside yarem Vienna And promote so that the end of the catheter is in the cranialist Vienna at the right atrium. The three-way crane through the extension tube is attached to the catheter, the system for the introduction of the liquid and the pressure gauge. The pressure gauge is vertically fasten on the wall of the animal cell in such a way that the "zero" of the pressure gauge was located at about the end of the catheter and the right atrium. With the patient's position on the stomach, this level is approximately 5-7.5 cm above the sternum on the fourth intercostal. In the position of the animal on the side of the zero mark parallel to the chest in the 4th segment area. The FED is measured by filling the pressure gauge isotonic crystalloid solution and the subsequent disconnection of the tank with the liquid using the locking crane. This procedure allows you to equalize the pressure of the fluid column in pressure gauge and blood in the catheter (vein). The mark on which the liquid column will stop in the pressure gauge when the pressure is equalized, and is the magnitude of the pressure in the cranial hollow vein.
11. What are normal values FVD?
Dogs 0-10 cm Water.st.
Cats 0-5 cm waters. Art.
Single measurements of the CTC far from always reflect the state of hemodynamics. Repeated measurements and analysis of trends in comparison with the treatment carried out are more informative to estimate the volume of blood, the function of the cardiovascular system and the vascular tone.
12. Who is the monitoring of the FED?
FED measurements allow control of liquid therapy in animals with poor perfusion, circulatory failure, lung diseases with pulmonary hypertension, a decrease in total vascular resistance, increased permeability of capillaries, heart failure or impaired kidney function.
13. What are the critical values \u200b\u200bof the CVD?
The value of the CVD (see Water. Art.)
Interpretation
The patient needs fluid introduction. If there are signs of vasoconstriction or hypotension, the bolus injection of the fluid is recommended to reach the level of FLA 5-10 cm. Art.
Normal values.
Liquid therapy must be stopped; Probably violation of the heart function. At high values \u200b\u200bof the FLA, observed constantly, in combination with vasoconstriction or hypotension, assume heart failure.
Invasive (direct) method of measuring blood pressure applies only in stationary conditions when surgical interventionsWhen the injection of the patient's patient with a pressure sensor is necessary for continuous control of the pressure level.
The sensor is introduced directly into the artery. , Direct manometry is almost the only method of measuring pressure in the cavities of the heart and central vessels. The advantage of this method is that the pressure is measured constantly, displaying in the form of a pressure curve / time. However, patients with invasive monitoring hell require constant surveillance due to the danger of development. heavy bleeding In the case of disconnecting the probe, the formation of hematoma or thrombosis at the point of puncture, attachment of infectious complications.
Bloodstock speed
The speed of blood flow, along with blood pressure, is the main physical value characterizing the state of the circulatory system.
There are linear and volumetric speed of blood flow. Linear The speed of blood flow (V-lin) is the distance that the blood particle passes per unit of time. It depends on the total area of \u200b\u200bthe list of all vessels, forming a segment of the vascular bed. Therefore, in the circulatory system, the most wide plot is aorta. Here the highest linear blood flow rate, which is 0.5-0.6 m / s. In the arteries of the middle and small caliber, it decreases to 0.2-0.4 m / s. The total lumen of the capillary channel is 500-600 times less than the aorta, so the rate of blood flow in capillaries is reduced to 0.5 mm / s. Slowing the current of blood in the capillaries has a lot of physiological significance, as they occur in them there is a transcapillary exchange. In large veins, the linear rate of blood flow increases to 0.1-0.2 m / s. The linear speed of blood flow in the arteries is measured by an ultrasound method. It is based on the Doppler effect. The sensor with the source and the ultrasound receiver will be prevented on the vessel. In a moving medium - blood, the frequency of ultrasonic oscillations changes. The greater the blood flow rate along the vessel, the lower the frequency of reflected ultrasound waves. The speed of blood flow in capillaries is measured under a microscope with fission divide, by observing the movement of a certain erythrocyte.
Volume The speed of blood flow (volume) is the amount of blood passing through the cross-section of the vessel per unit of time. It depends on the pressure difference at the beginning and end of the vessel and the flow of blood. In the clinic, bulk bloodstream is estimated by renowview. This method is based on the registration of the oscillations of electrical resistance of organs for the current of high frequency, when they change their blood flow into systole and diastole. With increasing blood flow, the resistance decreases, and the decrease increases. For the purpose of diagnosis vascular diseases produce renowmography of limbs, liver, kidney, chest. Sometimes use plentomography. This is the registration of oscillations of the volume of the organ arising from the change in their blood flow. Volume oscillations are registered with the help of water, air and electric padsmographs.