The best antibiotic for adults at pneumonia. Pneumonia: Antibacterial therapy
Antibiotics are a group of drugs with which you have to face or another to almost every person. Despite the fact that these drugs are considered severe, without them, unfortunately, it is impossible to do - in particular, in the treatment of pneumonia. What antibiotics when inflammation of the lungs are used especially often and why they are the most effective means to combat this disease, we will discuss in the article.
What factors affect the choice of a particular medication when inflammation of the lungs?
In medicine, pneumonia refers to a group of severe and life-threatening patient ailments. Viruses and fungi may be causative agents. But most often, the disease is infected with bacteria - pneumococci, streptococci, staphylococci, etc. The lung site ceases to function normally, causing many severe consequences for the body.
Not so long ago, the main antibiotics to combat the inflammation of the lungs were easy to determine, since this ailment was treated only by the preparations of a penicillin row. But, as it turned out, the bacteria are able to produce resistance to drugs. Now named antibiotics may already be as effective, researchers had to develop new drugs. Nowadays, there have been a huge amount of their quantity, as well, and at the same time difficult for a doctor, since now he has to take into account the mass of factors to choose adequate treatment.

What antibiotics when inflammation of the lungs will be appointed, now depends on many points: not only the form of the disease, but also its causes, the susceptibility of the body to this drug, as well as what drugs of this group have already been used to be patients earlier.
How do you prescribe treatment at pneumonia?
In order for the diagnosis to be as accurate as possible in the composition of the patient's sputum laboratory, the type of bacteria provoked the disease. In decoding the analysis, as a rule, the pharmacological group is indicated, and among its drugs, the doctor selects what the least of all contraindications and side effects. In this case, it is mainly about the following:

Each of them includes active substances that allow a specialist to most accurately choose that antibiotics are appropriate on the basis of a particular case, and to expand the scope of the drugs, it is quite often necessary to assign funds directly from two groups.
The use of antibiotics depending on the causative agent
It's not so difficult to guess that each of the listed series is best copes with certain types of pneumonia pathogens. Thus, macrolides are best acting on the activity of pneumococci, provoked inflammation of the lungs. Treatment with antibiotics from a group of fluoroquinolones in this case turns out to be ineffective, and microorganisms are practically insensitive to drugs of tetracycline series.

For hemophilic sticks, drugs from fluoroquinolones are most active, and if the disease is caused by enterobacteria - preparations from the group in the treatment of mycoplasma or chlamydial pneumonia are chosen, as a rule, macrolides and antibiotics from the tetracycline group.
What antibiotics are most often applied
Of course, in medical practice, there are antibiotics, with inflammation of the lungs, the most popular with doctors. So, if the patient has not reached 60 years, he does not have sugar diabetes or pathologies of cardio-vascular system, for the treatment of segmental or focal pneumonia, experts prefer perfectly proven drugs "Aveloks" and "Tavanik" (which, by the way, is preferable than its more cheap analog Loksof or Levofloxacin). If they are taken in combination with "Amoxiclav" or "Augmentin" tablets, then a positive effect can be achieved in two weeks after the start of reception.
If the patient's condition does not improve, and the temperature does not fall even on the fourth day, then other antibiotics against lung inflammation should be selected. As a rule, in such cases, the drugs "Azitro-Sandoz" or "Sumamed" instead of "Augmentin" are prescribed.

A good combination is also considered to use Tablets "Sumamed" (1 tab. 1 time per day) in combination with intramuscular or preparation "Fortum" (2 mg 2 times a day).
Popular injections: Antibiotics when inflammation of the lungs
The course of antibiotic injections at pneumonia is usually from seven to ten days. But in no case, this treatment cannot be carried out independently, without appointing and observing the doctor, or interrupt the prescribed course, deciding that the well-being has already improved. All this eventually provokes resistance to drugs from surviving bacteria, and the trouble-free or returned pathology will be more complicated, while it is worse to treat treatment.
Most often, the following antibiotics are used in the form of injections when inflammation of the lungs:

By the way, it should be noted that when appointing antibiotics there are several features. So, the conclusion that you need to replace this drug can only be made in 2-3 days after the start of treatment. The reason for such a decision may be the risk of serious side effects or excessive toxicity of any antibiotic that will not allow their long time.
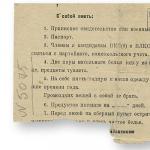
Basic rules when carrying out injections from pneumonia
Effective antibiotics can only pick up the doctor. But if the patient is shown, then to make it injections will have to someone from loved ones. In this case, not to cause unnecessary complications, several rules should be followed.
- Remember that the course of treatment with an antibiotic in pneumonia cannot be less than 10 days.
- When prescribing drugs for injections that are produced in the form of powders, remember: it is possible to breed them only before the procedure. Do not do it in advance!
- For physiological saline, novocaine, lidocaine or water for injection are used. They are taken in the standard proportion: per 1 g of the drug - 1 ml of liquid.
- Before the first prick, make skin sample. To do this, scratch the sterile disposable needle from the syringe of the skin and apply a few drops of the assigned tool to the wound. If after 15 minutes it was not blushing and did not get it, then there is no allergies for this medicine. Otherwise, it needs to be replaced.
- If a painful infiltrate remains after injections - it is applied to it to accelerate the resorption.
What antibiotics refer to backup
In the case of severe pneumonia, the patient is prescribed so-called reserve drugs. That is, potent antibiotics, which are "left" by doctors on extreme case (All this is done due to the easily generating stability of bacteria to drugs).

Therefore, it is worth remembering their name. Antibiotics when inflammation of the lungs with a heavy flow is "Ceftazidim", "Timenin", "Sparfloxacin", "Tientam", "Grimipen". They are not prescribed in the case of a light or moderate severity of the disease, because no one is insured in the future from operational interventions And the likelihood of health, when their application will be especially necessary.
What antibiotics should not be used
In view of the previously mentioned high resistance to drugs of microorganisms, which caused inflammation of the lungs, the treatment of antibiotics listed below will not give the desired effect. To such means include:
- simple penicillins ("biotelin", "ampicillin", "oxacillin", etc.),
- cephalosporins of the first and second generation ("Cefazolin", "Cefalexin", "Cefamisin"),
- fluoroquinolones of the first and second generation ("Nalidix Acid", "Norfloxacin", "Ofloxacin" and "Ciprofloxacin").
Do not assign yourself antibacterial therapy!
Finally, I want to emphasize that it is very dangerous to apply antibiotics yourself, but not only because they can cause serious side effects.
Regardless of what antibiotics are inflammation of the lungs, microorganisms very quickly produce drug resistance to them. So, every new case in which these drugs will have to take, threatens that the expected action will not occur. This, of course, will tighten the course of the disease and cause various difficulties. Therefore, so as not to put yourself in the future in a difficult position, do not self-medicate. And be healthy!
Beta-lactam penicillin antibiotics amoxicillin + clavulanic acid (drugs with names - Augmentin, Flemoclav Solutab) are served. Antibiotics are released in tablet form, which allows them to use them to appoint a doctor at home and for children.
The inflammation of the lungs is caused by the pathogens of several groups. Especially often community-hospital pneumonia (which occurred outside the hospital walls, in contrast to the hospital infection) provoked Streptococcus Pneumonia, Haemophilus Influenza, Staphilococcus Aureus, Pseudomonas Aeroginosa and other simplest, among whom Mikoplasm, Legionells, Chlamydia.
A single antibiotic capable of acting equally effectively on all causative agents of inflammation of the lungs does not exist, for each type of infection, the most effective drug is selected empirically.
For the treatment of pneumonia, several groups of antibiotics are used:
- beta lactam;
- macrolides;
- tetracyclines;
- fluoroquinolones.
It is impossible to distinguish which when inflammation of light antibiotics are the best, and which are ineffective, since in each case the result of treatment is determined not only by the type of pathogen of pneumonia, but also the reactivity of the immune system, concomitant chronic diseases, care characteristics.
Beta-lactam antibiotics
Beta-lactam antibacterial agents are used by the main drugs for the treatment of pneumonia, combined on the basis of the presence of a beta-lactam ring molecule.
The means have a similar mechanism of action, differ in sensitivity to the enzymes of beta lactamases, which are produced by bacteria.
High efficiency against pneumococci, often causing pneumonia, are distinguished by amoxicillin antibiotics, in the absence of allergies to the drug selection in children and during pregnancy.
Beta-lactam includes:
- penicillins;
- natural - benzpenicillin, oxacillin;
- ampicillin;
- - Hikcotl, Flexin Soluteab;
- inhibitory-speaking - Augmentin, Timemitin;
- antsingenic ureidopenicillars - azlocillin, pepactorin;
- cephalosporins;
- 1 generation - cefazolines (Cefzol, Cefhamesein), cephalexin;
- 2 generation - means with cefuroxime (zinnat, keticef);
- 3 generation - cefotaxim (clafranoran), ceftriaxone (Rosethim), Ceftazidim (Fortum);
- 4 generation - cefepim (maxim).
Beta-lactam antibacterial agents are characterized by high efficiency, but are able to cause allergies, which is why they are replaced by macrolides or fluoroquinolones. Macrolids - Preparations of choice when suspected atypich formwhich causes chlamydia, legionells, mycoplasma.
To the benefits of these antibacterial agents There is a significant additional libeotic effect in which a high concentration of the drug is created in the blood, which remains in the therapeutic dose after the discharge of the drug.
For example, azithromycin is a post-libeotic effect of 4 days, which reduces the course of therapy to 5 days.
Features of community-hospital pneumonia
 Inflammation of the lungs can develop rapidly without leaving time to hold diagnostic studies On the definition of pathogenic microflora. The first appointment of the antibiotic and in private clinicAnd in the State Hospital is made empirically.
Inflammation of the lungs can develop rapidly without leaving time to hold diagnostic studies On the definition of pathogenic microflora. The first appointment of the antibiotic and in private clinicAnd in the State Hospital is made empirically.
Choosing which antibiotics to take, the doctor comes from clinical picture Diseases, prevalence of pneumonia pathogens in a given area, the most typical pathogens, presence in the history of chronic diseases in adults.
The treatment of inflammation of the lungs is carried out by tableted forms, penicillins and cephalosporins 2 generations are served by the preparations of choice. To the appointment of treatment in the form of injections, it is impossible for the impossibility of treating tablets, as well as with severe disease.
Thus, the hospital forms of pneumonia in adults are read to treat with the introduction of antibiotics in injections, and go to the reception of the tablets only on 3 days after the element of the symptoms of inflammation.
Treatment of pneumonia in adults
The effectiveness of the antibiotic is estimated after 3 days from the start of therapy. During this time, the necessary therapeutic concentration is created in the blood, and the medication acts with the maximum result.
With a non-heavy flow of pneumonia caused by pneumococcal, streptococci, use drugs for receiving inside containing:
- amoxicillins - amoxicillin Sandoz, Flexin Solutub, Hikcotil, Amosin, Ospamex - 0.5 g at intervals at 8 o'clock;
- amoxicillins + Clawulanate - Augmentin, Bethaclav, Flemoclav Soluteab, Ecoclav, Amoxiclav - 0.65 g, Intervals - 8 hours;
- Cefuroxime Axietyl - dosage 0.5 g, intervals - 12 hours.
In the absence of a result after 3 days of use, probability, adults are prescribed:
- tetracyclines - doxycycline inside 0.1 g at intervals at 12 o'clock;
- macrolids:
- clarithromycin - Clasid, Frozilide, FROMILID UNO, Romiklar, Clarithromycin Sandoz, Clarbact 0.5 g at intervals at 12 o'clock;
- azithromycin - Sumamed, Azitral, Hemomycin, Zitrolid Forte, Azitrumycin Zentiva, Azithoks, Ztorilla 0.5 g 1 day once, the following days - 0.25 g 1 time per day;
- midekamicin - Macroin 0.4 g after 8 hours;
- spiramycin - Spiramycin-Vero, Rovamycin of 3 million meters at intervals at 12 o'clock;
- roxitromycin - Brillide, Rulid, Rulicin, Esparoxy 0.15 after 12 hours;
- erythromycin - 0.5 g with intervals of 6 hours of erythromycin tablets;
- josamamicin - Vilplerafen, Vilplephen Soluteab 0.5 g with an interval of 8 hours;
- Fluoroquinolones:
- gatifloxacin - Zharkov, Gatispan 0.4 g 1 time / day;
- levofloxacin - Tavanik, Flexide, Floracide, Leo Auto, Glewo 0.5 g 1 time per day;
- moxifloxacin - Aveloks, Hainemox 0.4 g 1 time / day.
Pneumonia in the elderly
With pneumonia in adults after 65 years, with a non-heavy form of leakage from the first day of treatment, protected aminopenicillins of Augmentin or amoxyclav, axietyl cefuroxime or one of the fluoroquinolones in the usual dosage are prescribed.
Alternative preparations for older patients serve doxycycline or cefaclor.
Pneumonia during pregnancy
 During the pregnancy of women sick pneumonia, they definitely hospitalize. Antibacterial drugs are used in pregnant women only by testimony.
During the pregnancy of women sick pneumonia, they definitely hospitalize. Antibacterial drugs are used in pregnant women only by testimony.
Choose for the treatment of medicine possessing maximum effectBut do not harm the emerging fetus.
To allow for pregnancy antibiotics for the treatment of pneumonia include:
- amoxicillins - Table. 0.5 g with intervals at 8 o'clock;
- amoxicillin + clavulanate - after 8 hours;
- cefuroxime Axietyl - 0.5 g with an interval of 12 hours;
- ampicillin - in injection 1 g after 6 hours;
- ceftriaxone - in injection 1 g at intervals of 24 hours;
- ceffaxim - in the injection of 1 g at intervals at 8 o'clock;
- cefuroxime - injection 1.5 after 8 hours.
An alternative preparation for allergies to beta-lactam penicillins in pregnant women is a spiramycin, which is prescribed to intake in 12 hours in suspension of 3 million meters.
Heavy pneumonia
With severe flow complete Pneumonia Prescribed cefepim, ceftriaxone or cefotaxim as a drug selection. In addition to the main drug, an antibiotic from the group of macrolides is clarithromycin, spiromycin or erythromycin.
The most severe flow of lung inflammation is noted when infected with staphylococcus, pneumococci, enterobacteria, legionells. With severe forms of inflammation, drugs are injected intravenously, pairs of drugs are used:
- amoxicilling + clavunate and macrolide injection;
- cefotaxim + macrolide;
- ceftriaxone + macrolide;
- ciprofloxacin (offloxacin) + cephalosporin 3 generations (or levofloxacin, moxifloxacin).
Replacing antibiotics
 The effect of the use of the antibiotic is to reduce the symptoms of intoxication, reducing the temperature. If this does not happen after 3 days, then the drug is replaced.
The effect of the use of the antibiotic is to reduce the symptoms of intoxication, reducing the temperature. If this does not happen after 3 days, then the drug is replaced.
An ampicillin can often serve as a choice, in the absence of a result, it is replaced by a macrolide or attach it to add. And with severe pneumonia, instead of ampicillin use macrolide + one of the cephalosporins of 3 generations.
If amoxicillin or cefuroxime, amoxicillin or cefuroxime were prescribed to the patient, then the drug from the group of macrolides is attached to it.
The reason for changing the antibiotic can be developing renal failure In the patient, due to the nephrotoxicity of the drug. Nephrotoxic drugs include cephalosporins, fluoroquinolones.
How many therapy lasts
Subject to the normalization of temperature for 4 days, the total duration - 7-10 days. The duration of the course with mycoplasma pneumonia is 2 weeks.
When infecting enterobacter, staphylococci, legionells, the treatment course can be extended to 3 weeks.
Criteria recovery
Signs of the normalization of the patient's condition serve:
- decrease in temperature to values \u200b\u200bnot exceeding 37.5 0 s;
- reduction of breathing frequency up to 20 and less breathing per minute;
- lack of pus in sputum;
- reducing the signs of intoxication of the body.
The use of antibiotics is important, but only one goal is to destroy the infection. The tasks of restoration of lung functions solve drugs from other groups - anti-inflammatory, expectorant, the overall result of treatment depends on the correctly selected treatment, age, immunoreactivity of the patient.
Pneumonia is one of the most dangerous infectious diseases of the respiratory tract (respiratory tract), which is characterized by the defeat of the lower respiratory tract (alveol) and lung parenchyma. The main principle of its treatment (as well as at bronchitis) is antibiotic therapy - that is, treatment aimed at elimination of the pathogen (that is, the defeat of the microorganism, which led to inflammation of the lungs).
Without use of antibiotics with pneumonia, it is almost impossible to cure the patient, since rare the immune system Correct with pneumonia yourself. All other approaches and techniques (treatment with probiotics, expectorant drugs, disinfecting therapy, antipyretic drugs and all so many) are exclusively auxiliary character, as at bronchitis. It is important to understand - using only antibiotic therapy, it is possible to cure pneumonia, although with side effects, very unpleasant, unpleasant. Without an antibiotic - pneumonia is incurable, unlike bronchitis, and the likelihood of death, especially in a child.
Not in vain before the invention, penicillin Fleming, the inflammation of the lungs was one of the most common causes of mortality. It is fair to say that the invention of antibiotics is a new word in medicine, which has been relevant to a qualitatively new level. No homeopathic or an Aüverdic drug can compare with the effectiveness of antibiotics, despite all the promotion that some pharmaceutical companies are satisfied.
So, what groups are classified antibiotics at pneumonia and with bronchitis, which of them are applied in the treatment of pneumonia? This question is ambiguous, since, by and large, representatives of absolutely all pharmacological groups are applicable in the treatment of lung inflammation. However, in the absolute, overwhelming majority of cases, the following groups of antibiotics from pneumonia are used:
This includes penicillins, cephalosporins and carbapenes. The most proven representatives of these subgroups are as follows:
- Cephalosporins wide spectrum actions. There are four generations of cephalosporins of a wide range of action.
- Penicillins (unprotected and protected forms, which are characterized by the presence of resistance to beta lactamases - enzymes allocated for the purpose of protection of bacteria) - OSPAMOKS, Augmentin, Amoxiclav, Sulbactam, ampicillin.

- The carbapenes of the wide range of action - measurement, imipenem.
Group of macrolides
Antibiotics from pneumonia and bronchitis of a wide range of action produced exclusively in oral form. Well-proven antibiotics for pneumonia, long known in the domestic and foreign pharmaceutical market. It should be noted that for some time the growth of microorganisms resistance to these antibiotics is due to improper diagnosis and non-compliance with the steps of therapy, however, today the most modern forms of macrolides act well. The most famous and effective representatives today are azithromycin (Ziomycin, Sumamed, Azicin Darnitsa, Ormax, Azitro-Sandoz), Clarithromycin (Clacian), Rovamycin (Roxylide).
Fluoroquinolones
This is a group of antibiotics from pneumonia and bronchitis of a wide range of action, which has its own niche of use. It is used mainly as a reserve preparation, if there are contraindications to all other groups. The most frequently used subgroup is the third-generation respiratory fluoroquinolones, the most famous representative - Levofloxacin (Tigeron, Eleflox); Fluorochinolones of the fourth generation are also used - Ozerlik. Ciprofloxacin has more proven itself as a drug of choice in the treatment of all sorts of intestinal infectionsAlthough with pneumonia will also help effectively cure and cure. 
A group of antibiotics from pneumonia and bronchitis - aminoglycosides. Are considered to prepare reserve. As a rule, applied against the amikacin pneumonia or gentamicin. Incredible effective drugsBut cause severe side effects.
Glycopeptides.
A group of antibiotics from pneumonia and bronchitis - glycopeptides. Vancomycin is the strongest antibiotic, used against pneumonia only in the resuscitation and intensive therapy.
In which clinical case, what antibiotic is better to assign?
There are several specific rules according to which antibiotics are prescribed for pneumonia, bronchitis and other infectious diseases:

Tactics of patients in each individual case
These are all general rules and algorithms for treatment with antibiotics of pneumonia and bronchitis (and actually as all other infectious diseases). However, often falls in practice to move away from these generally accepted standards and choose other antibiotics when inflammation of the lungs, especially if you have to be treated at home.
To begin with, let's look at the outpatient (polyclinic practice). It turns on to receive a patient with complaints of an increase in temperature to febrile values, a strong cough with a large amount of sputum. Auscultatively listens to the abundance of wet wheezing in the lower lungs, percussion - the dullness of the sound above one of the areas. Plus - classical symptoms in the form of intoxication, catarrhal manifestations. Yes, this patient has no picture of the survey radiographic organs chestno, and the next week there will be no sowing of sputum with the determination of the sensitivity of microorganisms to antibiotics, not even ready general analysis urine and blood. However, it is already right now it is necessary to begin empirical therapy with antibacterial preparations of a wide range of action. Even if suddenly the diagnosis of pneumonia is not confirmed and there will be ordinary bronchitis - it will still have to use an antibiotic. So the tactics of keeping will not change.
What kind of antibiotic at pneumonia it is better to choose? Good question. It is necessary to repel solely on what characteristics the patient has and where we will treat it. Important remark - only the light shape of pneumonia at the very responsible, adult patient can be treated in outpatient conditions, that is, at home. Nevertheless, other cases sent to the hospital.
 In the case of treatment at home, Augmentin 1000 mg will be used at the rate of one tablet three times a day, with an interval of eight hours, a course for seven days. If the patient has the opportunity to do intramuscular injection at home - it is better to prescribe Ceftriaxone intramuscularly, one gram twice a day with an interval of twelve hours (again, a small deviation from treatment standards, but in this case it is reasonable, since Augmentin loses its effectiveness with each day). In case of suspected atypical etiology, a macrolide is azithromycin or clarithromycin on one tablet once a day, a course for three to five days, depending on the severity of the state. The appointment of fluoroquinolones is not excluded (for example, if the patient was detected allergic to beta - lactams) - then it will be possible to take 500 mg levofloxacin light inflammation, drinking one tablet once a day, a course for five days, regardless of , at home or in the hospital.
In the case of treatment at home, Augmentin 1000 mg will be used at the rate of one tablet three times a day, with an interval of eight hours, a course for seven days. If the patient has the opportunity to do intramuscular injection at home - it is better to prescribe Ceftriaxone intramuscularly, one gram twice a day with an interval of twelve hours (again, a small deviation from treatment standards, but in this case it is reasonable, since Augmentin loses its effectiveness with each day). In case of suspected atypical etiology, a macrolide is azithromycin or clarithromycin on one tablet once a day, a course for three to five days, depending on the severity of the state. The appointment of fluoroquinolones is not excluded (for example, if the patient was detected allergic to beta - lactams) - then it will be possible to take 500 mg levofloxacin light inflammation, drinking one tablet once a day, a course for five days, regardless of , at home or in the hospital.
In the case of inpatient treatment of pneumonia or bronchitis, it is immediately necessary to use injection forms of antibiotics at pneumonia in adults. If there is a common, extractive pneumonia - you can completely dispense with antibiotics at pneumonia in adults, like ceftriaxone, zinacef or cefoperazone. In the event that there is a suspicion of the hospital infection (the same cinema stick) - recommended by cefepim.
And if the meticillin-resistant staphylococcus (MRSA) was sigh of (MRSA) - it is necessary to use the most powerful antibiotics - aminoglycosides, carbapenes or glycopeptides. To date, the most powerful antibiotic treatment circuit is a combination of Tianship + Vancomycin + amikacin - it overlaps all the famous science of microorganisms.
Regarding the use of antibiotics in children - the difference is the dosages and in the fact that many groups of antibacterial drugs in childhood Not applicable. At home, fighting inflammation of the lungs is also too risky. In children, only penicillins, cephalosporins and macrolides can be used. All other groups are exclusively on life indications and in cases where the expected benefit exceeds a possible risk.
conclusions
Antibiotic therapy is a serious direction in therapy, and therefore to treat at home the pneumonia is still better not worth it. If only because injections will have to do intravenously, intramuscularly - and at the same time you can apply infection.
Video: Rehabilitation after antibiotics - the school of Dr. Komarovsky
Inflammation of the lungs is a disease that is found in both adults and completely small children. The causative agents are viruses, bacteria, other microorganisms. The main danger that can be expected from this ailment is extremely difficult the physical state And even the fatal outcome. That is why therapy should be timely. Mainly practiced the treatment of pneumonia with antibiotics.
How pneumonia develops. Classification
Most often, this disease occurs due to the pathogenic microflora in the respiratory tract: staphylococci, pneumococci, legionell, intestinal sticks and others. In this case, inflammatory processes are developing in the tissues of respiratory organs. Also inflammation of the lungs can be provoked and viral infections, and some toxic substances, rarely pneumonia is a consequence of the injury of the chest. There is a group of risk in which smokers, people who abuse alcohol, patients, long in bed mode, as well as older ages. Depending on the type of pathogen, bacterial, viral, fungal and mixed pneumonia distinguish. If one light is hit, then they talk about one-sided inflammation. There may also be bilateral, total, equity, segmental pneumonia. Depending on epidemiological data, the disease is a non-hospital, non-hospital, atypical nature, as well as an immunodeficial state.

Basic symptoms of illness
One of the main symptoms in the development of inflammatory processes in the lungs is cough. Also, with breathing, characteristic pain can be felt, the breathrick appears. Especially sharply appear pain in deep breaths, cough. With pneumonia, a high body temperature is observed. However, not always inflammation of the lungs is accompanied by its increase. The patient feels weakness throughout the body, fatigue, decreases appetite, is nausea and even vomiting. Symptoms in older people and children appear especially difficult. All this suggests that to facilitate the state and in order to avoid the development of complications, it is necessary to start taking antibiotics at pneumonia. This disease has a feature: antibacterial drugs are prescribed immediately, without waiting for laboratory research. After receiving the results of the analysis of sputum treatment is adjusted.
Disease flow stage
Experts identify three severity of inflammation of respiratory organs. Easy stage is characterized by poorly pronounced intoxication, the body temperature is within 38 ºС, the heartbeat is not accelerated. At the same time, a person retains clear consciousness. With a radiographic study, a small affected area is detected. With a more severe degree, the temperature may increase to 39 ºС, intoxication is more expressed. Moderate tachycardia is observed, the sword appears. In X-rays, infiltration is pronounced brightly. The hardest degree is characterized not only by high temperature (up to 40 ºС), but also clouding the reason. A person can wander, the sword occurs even in a calm state. At the same time, the intricensation of the body is pronounced.
This group of drugs is aimed at the destruction of pathogenic flora. First of all, the specialist must suppress acute symptoms Diseases. In this case, antibiotics are prescribed, which have a wide range of action.

The doctor then sends a sample of a mocry to the laboratory. The results obtained are influenced by further treatment. A concrete pathogen is established, which provoked a disease. The specialist chooses the necessary antibiotic with pneumonia in adults, the action of which will be directed to the destruction of this microorganism. A combination of drugs is often required, since the pathogens may be several. For competent selection of drugs use an antibioticogram.
Antibioticogram
This analysis helps to determine whether the patient's body is sensitive to a specific antibiotic. After all, the market is saturated with all sorts of drugs, and often bacteria are the resistance to one type of drugs, but are destroyed under the action of the other. For the study you need a sick spree. The trial is affected by different drugs. During such an analysis, the most effective antibiotics are selected for pneumonia for a particular patient. They will suppress the growth of microorganisms. Weathequent drugs will not interfere with their development. The accuracy of this study is high. The only disadvantage is that it is necessary to wait a long time: they will be ready after 2-5 days.
Groups of antibiotics used in the treatment of pneumonia
The most often treatment of pneumonia antibiotics begins with the preparations of a wide range of action. These include penicillins, macrolides, tetracyclines, fluorochinols, aminoglycosides, cephalosporins.
Penicillins are one of the first antibacterial drugs. They are natural and semi-synthetic. Well penetrate into the fluid and tissue of the body. A number of unwanted phenomena are also called: diarrhea, hypersensitivity, allergic reactions. Treatment of pneumonia with antibiotics of this species effectively, if the pathogens are streptococci, staphylococci.
Tetracyclines are preparations that are used less often. The reason for this is the stability of microorganisms to their action. Also, the peculiarity of drugs lies in their ability to accumulate in bone tissues. At the same time, they can lead to the destruction of the teeth. Therefore, such antibiotics at pneumonia are not appointed pregnant women, women during breastfeeding period, children younger age, as well as patients who have kidney problems. Representatives of the drugs of the tetracycline group - "Doxycycline", "Tetracycline".

Cephalosporins group
There are 4 generations of this type of drugs. The first-generation drugs include "cefazolin", "cephalexin", etc. They actively act on the bacteria of the group of Cockkops (pneumococci, staphylococci). The second generation of drugs has good antibacterial properties in relation to both gram-positive and gram-negative flora. The half-resistance period is approximately 1 hour. Cephalosporins that belong to the third generation have an excellent effect on microorganisms that have resistance to the preparations of the penicillin group ("Cefotaxim", "Cefoperasazon"). Use them for the treatment of severe forms of infections. Cefepim is the name of antibiotics with fourth-generation pneumonia. They are most active. Among adverse Reactions After taking cephalosporins, the occurrence of allergy is most often distinguished. About 10% of patients note the presence of allergic reactions to these drugs.
Macrolids. Aminoglycosides
Macrolids are used to neutralize Cockkops, Legionella, Chlamydia. They are well absorbed inside the body, but the food intake slightly slows down this process. Allergic reactions observed very rarely. Representatives of this category are such drugs as "erythromycin", "azithromycin", "Clarithromycin". The main area of \u200b\u200btheir application is infectious processes in the respiratory tract. However, contraindications for receiving such drugs are violations in the liver.
Aminoglycosides - antibiotics at pneumonia, which actively affect aerobic gram-negative microorganisms. They also apply in cases where the disease is caused by not one type of bacteria, and therefore it is necessary to combine antibacterial drugs to achieve desired result. Group representatives are preparations such as "gentamicin", "amikacin". The dosage is calculated depending on the mass of the patient's body, its age, the severity of the disease. When taking such drugs, control of glomerular filtration in the kidneys is required.

Hinol and Fluorokinol class
Drugs of this category are divided by 4 generations. Nephorated (this is the first generation) actively affect the legionells, intestinal wand. Somewhat less they affect chlamydia, Cockki. First generation preparations are used for light infections. The remaining quinols (from the second to the fourth generation) are fluorid. All medications are well distributed in the body. Displays from the body mainly by the kidneys. The main contraindications to the application is the period of having a child, increased sensitivity to the drug. In addition, it is undesirable to use affected drugs to patients who have violations in the work of the liver, kidneys. Fluorochinols do not prescribe children (up to 18 years). An exception can only be the absence of an alternative option. This class includes such drugs as "Ciprofloxacin", "Pofloxacin", "Levofloxacin". Intravenously introduces drug data only drip.
What are the rules for the appointment of antibacterial drugs
If pneumonia is diagnosed, which antibiotics take, solves only a specialist. After the start of use of drugs, they are replaced by others. Indications for this are serious side effects that may occur in treating certain drugs. Also, the replacement occurs if the doctor does not observe the desired result (and the changes for the better should appear on the second or third day). Some antibiotics are pretty toxic. Therefore, their reception can not die for a long time. Basically, pneumonia treatment in adult antibiotics lasts 10 days. But more serious infections require a significantly larger period of time (about a month). The specialist should also take into account the overall condition of the patient, and the presence of certain concomitant and chronic diseases, man age. When appropriate antibacterial drugs, the possibility of creating a dose of drug in the blood is important, which will be sufficient precisely with this severity of the disease.

What forms apply antibiotics
Depending on the stage of the disease and severity of its flow, various ways of entering drugs are used. Basically in the first days of the disease, drugs are injected with injections. Cephalosporins (antibiotics for pneumonia) injections are produced intravenously or intramuscularly. This is possible due to their low toxicity. The feature of the macrolides is that they accumulate and continue to act even when the reception medicines stops. Light forms of the disease are treated in 10 days. In this case, antibiotics can be used with pneumonia in tablets. However, experts argue that the oral form of drug intake has not such high efficiency. This is explained by the fact that it is difficult to calculate accurate dosage. It is not recommended to change the drugs often, as this can develop the stability of microorganisms to antibiotics.
Features of the treatment of pneumonia in children
Especially dangerous inflammation of the lungs for young patients. There may be a disease even in kids. The main symptoms of pneumonia in small patients are wheezing, cough, difficult and frequent breathing, heat (which keeps pretty for a long time). It is worth paying attention to the behavior of the baby. He loses appetite, becomes sluggish, restless. The most important symptom of pneumonia in young children is the formation of a plot between lips and nose. As a rule, there is inflammation of the lungs as a complication after the transferred ORVI, and not as an independent disease. There are also congenital pneumonia (the pathogen - herpes virus, mycoplasma), infection can occur and directly during or after childbirth. In newborns, the respiratory tract is small, gas exchange is less intense. Therefore, the disease occurs harder.

Antibiotics and children
As with adults, the basis of therapy with inflammation of the lungs in kids is antibiotics. With pneumonia, children are entered by parenterally. This makes it possible to minimize the effects of drugs on the microflora of the digestive system. It is also possible to receive drugs in the form of injections or inhalations. The last method is most comfortable for young children. If the age of the child does not exceed 6 months, the treatment is carried out exclusively in the hospital, where the baby is under constant control of specialists. The course of therapy for children is 7 days in the case of taking drugs of the penicillin group, cephalosporins. If the doctor prescribed macrolides (this may be "azithromycin", "clarithromycin"), then the duration of treatment is reduced to 5 days. Antibiotics for pneumonia in children should show efficiency within 3 days. Otherwise, it is possible to replace the drug.
In no case cannot be engaged in self-medication. Even the best antibiotics at pneumonia, which helped one child, may be ineffective for another, and even dangerous. It is very important to strictly adhere to the graph of receiving medication. It is impossible to take synthetic vitamins and other immunomodulatory products in parallel. To prevent the occurrence of pneumonia, it is worth avoiding the undercooling of the body, in a timely manner to conduct therapy of colds and other infectious diseases. Don't forget about the right
Pneumonia - Heavy infectious diseasein which the lungs suffer. Despite effective medicationsFrom pneumonia die almost 10% of the number of all sick. Most people suffer from elderly, with weakened immunity, children.
With pneumonia, the causative agent of the disease falls into the lungs, begins inflammatory process In Alveola, spreading to other departments. Then the exudate appears (liquid secreted by small blood vessels With inflammation), respiratory failure arises, over time it can go to the heart.
The cause of infectious pneumonia may be:
- Bacterial infection, among its pathogens identify:
- Pneumococci and staphylococci;
- Gram-negative microorganisms hemophilic and intestinal sticks, legionella;
- Viral infections - herpes, adenovirus;
- Mushrooms.
- Non-infectious disease may occur:
- As an allergic reaction;
- Highly toxic poisoning;
- Due to injury in the chest area;
Atypical pneumonia - Another type of lung inflammation. It arises due to the impact of organisms, which are naturally similar to viruses at the same time, and on bacteria.
All types of lung inflammation have a number of identical symptoms and is the likelihood of incorrect diagnosis, which is why treatment can be appointed incorrect. Symptoms in inadequate treatment will increase - cough will increase, the overall state will deteriorate, even a fatal outcome is possible.
Therefore, it is important timely and proper diagnosis.
As a rule, the patient is hospitalized and immediately appoint a course of therapy - vitamins, enhanced nutrition, antipyretic drugs, but the main treatment is the use of antibiotics.

The antibiotic is a substance that overwhelming the growth of living cells is not used for the treatment of flu, hepatitis, measles, because it does not work for viruses. The antibiotic appeared in 1928, when the American scientist Alexander Fleming when conducting an experiment accidentally discovered the mold, which produced a substance that killing bacteria - he called it "Penicillin". In the USSR, Penicillin has improved the Soviet microbiologist Zinaida Yermoliev, in effectiveness it is one and a half times superior an imported analogue.
Purpose and treatment regimen
For the treatment of pneumonia, a scheme has been developed - antibiotics are prescribed at the initial stage - intravenously or intramuscularly. We need a sufficient concentration of the drug to more effectively combat the disease, then go to oral treatment.
- There is no laboratory conclusion about the causative agent of the disease, prescribe the preparations of a wide range of action, assuming the cause of the disease - sputum, temperature, temperature.
- An analysis is carried out to determine bacteria. As a rule, it takes at least 3 days.
- If necessary, treatment is adjusted, depending on the results of the study.
With a non-knowledge and moderate severity of pneumonia can be treated orally - Tablets or syrups (for children).
The result of treatment is noticeable after 4 days. If the effect of treatment is not observed, other antibiotics are prescribed.
This may be one of the funds:
amoxicillin, clavulanate, ampicillin, benzylpenicillin, cefotaxim, ceftriakon, as well as Levofloxacin or Moxifloxacin -intravenously or intramuscularly
After 4 days, if a positive effect is achieved, disappear clinical symptoms (The temperature is normalized, the cough and other signs decrease) are transferred to the oral use of the same drugs.
Remember! Antibiotics must be appointed only by the attending physician.
Treatment of severe pneumonia in adults
With a severe form of pneumonia, it is necessary to stay in resuscitation, as severe consequences are possible:

To prevent the development of complications, the combination of drugs is applied. Also, the basis for using combinations are:
- Heavy form of pneumonia.
- Low immunity.
- Infection pathogens are somewhat, which makes ineffective use of one drug.
- The occurrence of immunity to the drug.
Therefore, intensive treatment immediately prescribe, introducing intravenously combination of drugs:
- clarithromycin, erythromycin, spiramycin with antibiotica:
- amoxicillinor Clawulanate, Chasephim, Cefotaxim, Ceftriakson.
Alternatives - Levofloxacin Moxifloxacin Opleloxacin Ciprofloxacin with ceftaxim or ceftriaxone intravenously.
Important! Antibiotics are prescribed after careful diagnosis, individual treatment is selected to each patient, so in no case should engage in self-medication
In addition, the treatment of the phased, correctly choose the treatment regimen can only specialist, it depends on the causative agent of the disease, which is determined by the laboratory in wet and blood. This process can last more than a week, that is why the wide profile of antibiotics is used.
The duration of medication is 15-20 days.
Repeated treatment with antibiotics
If during 3 days the improvement does not occur, then treatment inefficient - Antibiotics are chosen incorrectly. Repeated analysis to clarify the pathogen, then corrected treatment. Other reasons for which the need for re-treatment arises:
- incorrect dosage;
- the patient was engaged in self-medication;
- prolonged treatment with antibiotics in which develops to a certain medicine;
- uncontrollable antibiotics reception, frequent change of the drug.
When the situation has arisen, some drugs are replaced by others - Tyarticillin, peperacillin.
Antibiotics with pneumonia in children
Treatment to children should be prescribed immediately when the symptoms are found.
Must be hospitalized:
- children up to 1 year, if the intrauterine infection is confirmed;
- children with congenital defects of the heart muscle and the circulatory system;
- children from orphanages, from families with bad socio-living conditions
- children with encephalopathy (damage to the structure and function of the brain);
- children under five, if he has detected a defeat more than one lobe of the lung;
- if the age of a child is less than two months;
- children with severe disease, regardless of age;
- children under two years with lobar (brunt) pneumonia;
- children are hospitalized if parents do not fulfill the recommendations of doctors.
Circuit diagram to obtain accurate results - Wide spectrum antibiotics, after laboratory research and detection of the pathogen, individual treatment is prescribed to each child, given the age of a small patient.
How to prescribe antibiotics to children
For doctors in the treatment of children, the age of a child is important. First, it depends on which the pathogens were the reason for the inflammation of the lungs and, secondly, not all drugs recommended Children.

- In newborn children frequent cause Diseases - streptococci groups in, intestinal wand listeriya.
- From 1 to 3 months - pneumococcus, golden Staphylococcus, Hemophilic wand.
- From 3 months to 5 years - Pneumococci and hemophilic stick.
- From 5 years most often pneumococci, mycoplasma, chlamydofila.
For the treatment of children due to the high drug sustainability of pathogens, such drugs do not apply:
1. Penicillin, Bicyllin oxacillin, ampicillin
2. Cephalexin Cefazolin Cefhamesein
3. NorFoxcin offloxacin.
In this regard, the treatment of newborn children under 3 months is carried out by amoxicillin with clavual acid. From this age, up to 5 years is possible treatment with tablets or syrup - macrolide or amoxicillin.
Older Children are treated by the same scheme.
The consequences of treatment with antibiotics
The use of antibiotics is necessary, including diseases such as inflammation of the lungs. But treatment has a side effect that depends on the dose of the received medication, from the duration of use. Which frequently encountered adverse reactions:
- disorders from the digestive tract - nausea, diarrhea, vomiting discomfort in the stomach;
- dysbacteriosis;
- allergic reaction - itching, rash, in severe case - anaphylactic shock, urticaria;
- candidiasis (thrush);
- anemia;
- hepatitis and pyelonephritis.
There are other side effects of antibiotics, especially if they were accepted for a long time, so doctors always warn:
Remember! self-medication is dangerous. You can harm yourself.
Prevention
The consequences after the use of antibiotics exist, of course, they are not always manifested, but it is better to prevent the disease, there are simple preventive measures for this.
- Food should be balanced - fruits, vegetables, meat and fish must be present in everyday diet.
- Make walkers in clean air, preferably in the park or forest.
- Throw bad habits - especially smoking
- Do not lead a sedentary lifestyle, moving more, to engage in physical education.
- Drink water at least 2 liters per day.
Preventive measures will protect against severe illness, but if the disease still appeared - it is necessary not to risk their health and if the diagnosis is pneumonia, be sure to treat antibiotics.